New Hematology Drugs
During the last two decades, we have witnessed the approval of numerous new hematology drugs and a complete transformation in how we approach blood cancers. A deeper understanding of the biology of specific hematologic malignancies has exposed numerous new therapeutic targets that were quickly followed by a plethora of novel therapeutic agents. The availability of novel drugs not only continues to improve patient outcomes but also generate numerous clinical questions. How to best combine or sequence new therapeutic agents? How to balance toxicity with the need for prolonged therapy? How cancer cells escape pharmacological suppression of a presumed vital pathway? How to make therapeutic innovations affordable to most patients? How to ensure barriers for clinical trial participation are removed so patients have early access to disease-modifying agents while answering the relevant clinic questions?
FDA Approved Drugs for Hematology
Drugs Approved in 2018
Andexxa (coagulation factor Xa (recombinant), inactivated-zhzo); Portola Pharmaceuticals; for the reversal of factor Xa inhibitors, Approved May 2018.
Andexxa (andexanet alfa) works by acting as a decoy for Factor Xa inhibitors in the blood, thereby preventing them from inhibiting the activity of native Factor Xa. As a result, the native Factor Xa is available to participate in the coagulation process and restore hemostasis (normal clotting).
Andexxa is specifically indicated for patients treated with rivaroxaban and apixaban, when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
Andexxa is supplied as a lyophilized powder for solution for intravenous injection. Dose Andexxa based on the specific FXa inhibitor, the dose of FXa inhibitor, and time since the patient’s last dose of FXa inhibitor. Administer as an intravenous (IV) bolus, with a target rate of 30 mg/min, followed by continuous infusion for up to 120 minutes. There are two dosing regimens: Low Dose: Initial IV Bolus: 400 mg at a target rate of 30 mg/min. Follow-On IV Infusion: 4mg/min for up to 120 minutes. High Dose: Initial IV Bolus: 800 mg at a target rate of 30 mg/min. Follow-On IV Infusion: 8mg/min for up to 120 minutes. Read more
Doptelet (avatrombopag); AkaRx; For the treatment of thrombocytopenia in adults with chronic liver disease scheduled to undergo a procedure, Approved May 2018.
Doptelet (avatrombopag) is a thrombopoietin receptor agonist.
Doptelet is specifically indicated for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure.
Doptelet is supplied as a tablet for oral administration. Begin Doptelet dosing 10-13 days prior to the scheduled procedure. The recommended daily dose of Doptelet is based on the patient’s platelet count prior to the scheduled procedure (see below). Patients should undergo their procedure 5 to 8 days after the last dose of Doptelet. Doptelet should be taken orally once daily for 5 consecutive days with food. In the case of a missed dose, patients should take the next dose of Doptelet as soon as they remember. Patients should not take two doses at one time to make up for a missed dose and should take the next dose at the usual time the next day; all five days of dosing should be completed.
Recommended Dose and Duration:
Platelet Count (x109/L): Less than 40 Once Daily Dose; 60 mg (3 tablets) for 5 days.
Platelet Count (x109/L): 40 to less than 50 Once-Daily Dose: 40 mg (2 tablets) for 5 days.
Lokelma (sodium zirconium cyclosilicate); AstraZeneca; For the treatment of hyperkalemia, Approved May 2018.
Lokelma (sodium zirconium cyclosilicate) is a highly-selective, oral potassium-removing agent.
Lokelma is specifically indicated for the treatment of hyperkalemia in adults.
Lokelma is supplied as a solution for oral administration. The recommended dose is 10 g administered three times a day for up to 48 hours. Administer Lokelma orally as a suspension in water. For continued treatment, the recommended dose is 10 g once daily. Monitor serum potassium and adjust the dose of Lokelma based on the serum potassium level and desired target range. During maintenance treatment, the dose may be up-titrated based on the serum potassium level at intervals of 1-week or longer and in increments of 5 g. The dose of Lokelma should be decreased or discontinued if the serum potassium is below the desired target range. The recommended maintenance dose range is from 5 g every other day to 15 g daily. Read more
Palynziq (pegvaliase-pqpz); BioMarin; For the treatment of phenylketonuria, Approved May 2018.
Palynziq (pegvaliase-pqpz) is a phenylalanine-metabolizing enzyme.
Playnziq is specifically indicated to reduce blood phenylalanine concentrations in adult patients with phenylketonuria who have uncontrolled blood phenylalanine concentrations greater than 600 micromol/L on existing management. Read more
Tavalisse (fostamatinib disodium hexahydrate); Rigel Pharmaceuticals; For the treatment of chronic immune thrombocytopenia, Approved April 2018.
Tavalisse (fostamatinib disodium hexahydrate) is a tyrosine kinase inhibitor with demonstrated activity against spleen tyrosine kinase (SYK).
Tavalisse is specifically indicated for the treatment of thrombocytopenia in adult patients with chronic immune thrombocytopenia (ITP) who have had an insufficient response to a previous treatment.
Tavalisse is supplied as a tablet for oral administration. Tavalisse should be initiated at a dose of 100 mg taken orally twice daily. After a month, if platelet count has not increased to at least 50 x 109/L, increase the Tavalisse dose to 150 mg twice daily. Use the lowest dose of Tavalisse to achieve and maintain a platelet count at least 50 x 109/L as necessary to reduce the risk of bleeding. Tavalisse may be taken with or without food. Read more
Drugs Approved in 2017
Aliqopa (copanlisib); Bayer; For the treatment of follicular lymphoma, Approved September 2017.
Aliqopa (copanlisib) is a kinase inhibitor with activity predominantly against the PI3K-alpha and PI3K-delta isoforms expressed in malignant B cells.
Aliqopa is specifically indicated for the treatment of adult patients with relapsed follicular lymphoma (FL) who have received at least two prior systemic therapies.
Aliqopa is supplied as a solution for intravenous infusion. The recommended dose is 60 mg administered as a 1-hour intravenous infusion on Days 1, 8, and 15 of a 28-day treatment cycle on an intermittent schedule (three weeks on and one week off). Continue treatment until disease progression or unacceptable toxicity. Read more
Besponsa (inotuzumab ozogamicin); Pfizer; For the treatment of adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia, Approved August 2017.
Besponsa (inotuzumab ozogamicin) is a CD22-directed antibody-drug conjugate (ADC).
Besponsa is specifically indicated for the treatment of adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia.
Besponsa is supplied as a solution for intravenous injection. Read more
Calquence (acalabrutinib); Acerta Pharmaceuticals; For the treatment of mantle cell lymphoma, Approved November 2017.
Calquence (acalabrutinib) is a small molecule Bruton tyrosine kinase inhibitor.
Calquence is specifically indicated for the treatment of adult patients with mantle cell lymphoma (MCL) who have received at least one prior therapy.
Calquence is supplied as a capsule for oral administration. The recommended dose is 100 mg orally approximately every twelve hours. The capsule should be swallowed whole with water and with or without food. Read more
Endari (L-glutamine oral powder); Emmaus Life Sciences; For the treatment of sickle cell disease, Approved July 2017.
Endari (L-glutamine oral powder) reduces oxidant damage to red blood cells by improving the redox potential of nicotinamide adenine dinucleotide (NAD), a coenzyme that has been identified as the primary regulator of oxidation.
Endari is specifically indicated to reduce the severe complications of sickle cell disease (SCD) in adult and pediatric patients age 5 and older.
Endari is supplied as a powder for oral administration. Read more
Giapreza (angiotensin II); La Jolla Pharmaceuticals; For the treatment of septic shock, Approved December 2017.
Giapreza (angiotensin II) is a vasoconstrictor to increase blood pressure in adults with septic or other distributive shock.
Giaprezza is specifically indicated to increase blood pressure in adults with septic or other distributive shock.
Giapreza is supplied as a solution for intravenous administration. Dilute Giapreza in 0.9% sodium chloride prior to use. See Full Prescribing Information for instructions on preparation and administration of injection. Giapreza must be administered as an intravenous infusion. Start Giapreza intravenously at 20 nanograms (ng)/kg/min. Titrate as frequently as every 5 minutes by increments of up to 15 ng/kg/min as needed. During the first 3 hours, the maximum dose should not exceed 80 ng/kg/min. The maintenance dose should not exceed 40 ng/kg/min. Read more
Hemlibra (emicizumab-kxwh); Genentech; For the prevention or reduction of bleeding episodes in patients with hemophilia A, Approved November 2017.
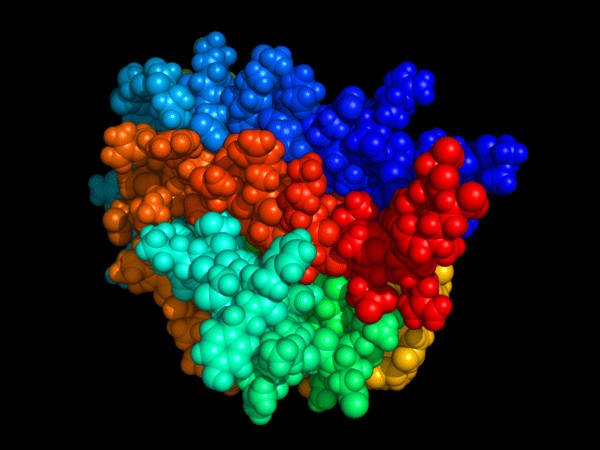
Hemlibra (emicizumab-kxwh) is a bispecific factor IXa- and factor X-directed antibody.
Hemlibra is specifically indicated for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adult and pediatric patients with hemophilia A (congenital factor VIII deficiency) with factor VIII inhibitors.
Hemlibra is supplied as a solution for subcutaneous injection. The recommended dose is 3 mg/kg by subcutaneous injection once weekly for the first 4 weeks, followed by 1.5 mg/kg once weekly. Read more
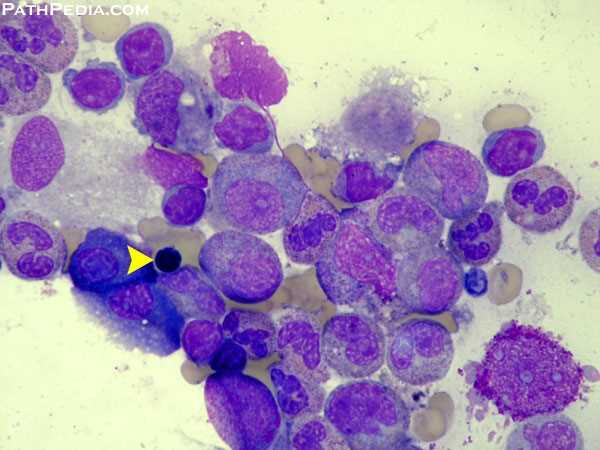
 IDHIFA (enasidenib); Celgene; For the treatment of relapsed or refractory acute myeloid leukemia with IDH2 mutation, Approved August 2017.
IDHIFA (enasidenib); Celgene; For the treatment of relapsed or refractory acute myeloid leukemia with IDH2 mutation, Approved August 2017.
IDHIFA (enasidenib) is a small molecule inhibitor of the isocitrate dehydrogenase 2 (IDH2) enzyme that works by blocking several enzymes that promote cell growth.
IDHIFA is specifically indicated for the treatment of adult patients with relapsed or refractory acute myeloid leukemia (AML) with an isocitrate dehydrogenase-2 (IDH2) mutation as detected by an FDA-approved test.
IDHIFA is supplied as tablets for oral administration. The recommended starting dose of IDHIFA is 100 mg taken orally once daily with or without food until disease progression or unacceptable toxicity. For patients without disease progression or unacceptable toxicity, treat for a minimum of 6 months to allow time for clinical response.
Do not split or crush IDHIFA tablets.
Administer IDHIFA tablets orally about the same time each day. If a dose of IDHIFA is vomited, missed, or not taken at the usual time, administer the dose as soon as possible on the same day, and return to the normal schedule the following day. Read more
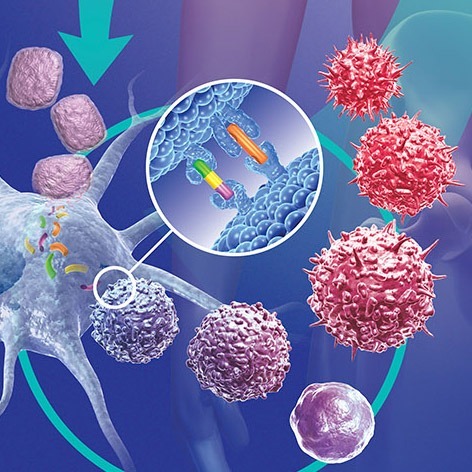
Kymriah (tisagenlecleucel); Novartis; For the treatment of refractory B-cell precursor acute lymphoblastic leukemia, Approved August 2017.
Kymriah (tisagenlecleucel) is a CD19-directed genetically modified autologous T cell immunotherapy.
Kymriah is specifically indicated for the treatment of patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
Kymriah is supplied as a suspension for intravenous infusion. Prior to infusion: premedicate with acetaminophen and an H1-antihistamine and confirm the availability of tocilizumab in the event of a CRS reaction. Dosing is based on the number of chimeric antigen receptor (CAR) positive viable T cells. For patients 50 kg or less, administer 0.2 to 5.0 x 10(6) CAR-positive viable T cells per kg body weight intravenously. For patients above 50 kg, administer 0.1 to 2.5 x 10(8) total CAR-positive viable T cells (non-weight based) intravenously. Read more
Rebinyn (Coagulation Factor IX (Recombinant), GlycoPEGylated); Novo Nordisk; For the treatment of hemophilia B, Approved June 2017.
Rebinyn is a proprietary glycopegylated recombinant factor IX for patients with hemophilia B. Rebinyn is specifically indicated for use in adults and children with hemophilia B for on-demand treatment and control of bleeding episodes and for the perioperative management of bleeding.
Rebinyn is supplied as a lyophilized powder for solution for intravenous injection. The recommended dose for on-demand treatment and control of bleeding episodes is 40 IU/kg body weight for minor and moderate bleeds, and 80 IU/kg body weight for major bleeds. Additional doses of 40 IU/kg can be given. The recommended dose for perioperative management: Pre-operative dose of 40 IU/kg body weight for minor surgery, and 80 IU/kg body weight for major surgery. As clinically needed for the perioperative management of bleeding, repeated doses of 40 IU/kg (in 1-3 day intervals) within the first week after major surgery may be administered. Frequency may be extended to once weekly after the first week until bleeding stops and healing is achieved. Read more
Rydapt (midostaurin); Novartis; For the treatment of FLT3 positive acute myeloid leukemia and mastocytosis , Approved April 2017.
Rydapt (midostaurin) is a multikinase inhibitor.
Rydapt is specifically indicated for the following:
- in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation chemotherapy, for the treatment of adult patients with newly diagnosed acute myeloid leukemia (AML) who are FLT3 mutation positive, as detected by a FDA approved test
- for the treatment of adult patients with aggressive systemic mastocytosis (ASM), systemic mastocytosis with associated hematological neoplasm (SM-AHN), or mast cell leukemia
Rydapt is supplied as a capsule for oral administration. Recommended Dosage in Acute Myeloid Leukemia: 50 mg orally twice daily with food on Days 8 to 21 of each cycle of induction with cytarabine and daunorubicin and on Days 8 to 21 of each cycle of consolidation with high-dose cytarabine. Recommended Dosage in ASM, SM-AHN, and MCL: 100 mg orally twice daily with food. Continue treatment until disease progression or unacceptable toxicity occurs.
Please see drug label for recommendations for dose modifications in patients with ASM, SM-AHN, and MCL. Monitor patients for toxicity at least weekly for the first 4 weeks, every other week for the next 8 weeks, and monthly thereafter while on treatment. Read more
Vyxeos (daunorubicin and cytarabine); Jazz Pharma; For the treatment of newly-diagnosed therapy-related AML or AML with myelodysplasia-related changes, Approved August 2017.
Vyxeos is a liposomal combination of daunorubicin, an anthracycline topoisomerase inhibitor, and cytarabine, a nucleoside metabolic inhibitor.
Vyxeos is specifically indicated for the treatment of adults with newly-diagnosed therapy-related acute myeloid leukemia (t-AML) or AML with myelodysplasia-related changes (AML-MRC).
Vyxos is supplied as a liposome for intravenous infusion. The recommended dose schedule is as follows: Induction: Vyxeos (daunorubicin 44 mg/m2 and cytarabine 100 mg/m2) liposome via intravenous infusion over 90 minutes on days 1, 3, and 5 and on days 1 and 3 for subsequent cycles of induction, if needed. Consolidation: Vyxeos (daunorubicin 29 mg/m2 and cytarabine 65 mg/m2) liposome via intravenous infusion over 90 minutes on days 1 and 3. Read more
Yescarta (axicabtagene ciloleucel); Kite Pharmaceuticals; For the treatment of relapsed or refractory large B-cell lymphomas, Approved October 2017.
Yescarta (axicabtagene ciloleucel) is a CD19-directed genetically modified autologous T cell immunotherapy.
Yescarta is specifically indicated for the treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, primary mediastinal large B-cell lymphoma, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma.
Yescarta is supplied as a suspension for intravenous infusion. Each single infusion bag of Yescarta contains a suspension of chimeric antigen receptor (CAR)-positive T cells in approximately 68 mL. The target dose is 2 × 106 CAR-positive viable T cells per kg body weight, with a maximum of 2 × 108 CAR-positive viable T cells. Read more
Drugs Approved in 2016
Afstyla (Antihemophilic Factor (Recombinant), Single Chain); CSL Behring; For the treatment of hemophilia A, Approved May 2016.
Afstyla (Antihemophilic Factor (Recombinant), Single Chain) is a recombinant, antihemophilic factor.
Afstyla is specifically indicated for use in adults and children with hemophilia A (congenital Factor VIII deficiency) for:
- On-demand treatment and control of bleeding episodes
- Routine prophylaxis to reduce the frequency of bleeding episodes
- Perioperative management of bleeding
Afstyla is supplied as a powder and solvent for reconstitution for intravenous injection. Please see drug label for recommended reconstitution and dosing schedules for each indication. Read more
Idelvion (Coagulation Factor IX (Recombinant), Albumin Fusion Protein); CSL Behring; For the treatment of hemophilia B, Approved March 2016.
Idelvion is a long-acting albumin fusion protein linking recombinant coagulation factor IX with recombinant albumin.
Idelvion was specifically approved for use in children and adults with hemophilia B for routine prophylaxis to prevent or reduce the frequency of bleeding episodes; on-demand control and prevention of bleeding episodes; and the perioperative management of bleeding.
Idelvion is supplied as a powder for solution for intravenous use after reconstitution only.
•One IU of Idelvion per kg body weight is expected to increase the circulating activity of Factor IX as follows:
- Adolescents and adults: 1.3 IU/dL per IU/kg
- Pediatrics (<12 years): 1 IU/dL per IU/kg
Administer intravenously. Do not exceed infusion rate of 10 mL per minute.
Control and prevention of bleeding episodes and perioperative management: •Dosage and duration of treatment with Idelvion depends on the severity of the Factor IX deficiency, the location and extent of bleeding, and the patient’s clinical condition, age and recovery of Factor IX. •Determine the initial dose using the following formula: •Required Dose (IU) = Body Weight (kg) x Desired Factor IX rise (% of normal or IU/dL) x (reciprocal of recovery (IU/kg per IU/dL)) •Adjust dose based on the patient’s clinical condition and response.
Routine prophylaxis: •Patients ≥12 years of age: 25-40 IU/kg body weight every 7 days. Patients who are well-controlled on this regimen may be switched to a 14-day interval at 50-75 IU/kg body weight. •Patients <12 years of age: 40-55 IU/kg body weight every 7 days. Read more
 Kovaltry [Antihemophilic Factor (Recombinant)]; Bayer; For the treatment of hemophilia A, Approved March 2016.
Kovaltry [Antihemophilic Factor (Recombinant)]; Bayer; For the treatment of hemophilia A, Approved March 2016.
Kovaltry is a recombinant, human DNA sequence derived, full-length Factor VIII concentrate. It temporarily replaces the missing clotting Factor VIII that is needed for effective hemostasis.
Kovaltry is specifically indicated for use in adults and children with hemophilia A (congenital Factor VIII deficiency) for on-demand treatment and control of bleeding episodes, for the perioperative management of bleeding and for routine prophylaxis to reduce the frequency of bleeding episodes.
Kovaltry is supplied as a powder for solution for intravenous use after reconstitution only. The recommended dose is as follows:
Control of bleeding episodes and perioperative management:
- Required dose (IU) = body weight (kg) x desired Factor VIII rise (% of normal or IU/dL) x reciprocal of expected/observed recovery (e.g., 0.5 for a recovery of 2 IU/dL per IU/kg).
- Estimated Increment of Factor VIII (IU/dL or % of normal) = [Total Dose (IU)/body weight (kg)] x 2 (IU/dL per IU/kg).
Routine prophylaxis:
- Adults and adolescents: 20-40 IU/kg 2 or 3 times per week.
- Children ≤12 years old: 25-50 IU/kg 2 times per week, 3 times per week or every other day. Read more
Opdivo (nivolumab); Bristol-Myers Squibb; For the treatment of classical Hodgkin lymphoma, Approved May 2016.
Opdivo (nivolumab) targets the cellular pathway known as PD-1/PD-L1, proteins found on the body’s immune cells and some cancer cells. By blocking this pathway, Opdivo may help the body’s immune system fight cancer cells.
Opdivo is specifically indicated for the treatment of patients with classical Hodgkin lymphoma that has relapsed or progressed after autologous hematopoietic stem cell transplantation (HSCT) and post-transplantation brentuximab vedotin.
Opdivo is supplied as a solution for intravenous administration. The recommended dose is 3 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity. Read more
Venclexta (venetoclax); AbbVie; For the treatment of chronic lymphocytic leukemia with 17p deletion, Approved April 2016.
Venclexta (venetoclax) is a BCL-2 inhibitor, an antiapoptotic protein.
Venclexta is specifically indicated for the treatment of patients with chronic lymphocytic leukemia (CLL) with 17p deletion, as detected by an FDA approved test, who have received at least one prior therapy.
Venclexta is supplied as tablets for oral administration. Initiate therapy with Venclexta at 20 mg once daily for 7 days, followed by a weekly ramp-up dosing schedule to the recommended daily dose of 400 mg. Venclexta tablets should be taken orally once daily with a meal and water. Do not chew, crush, or break tablets. Read more
Drugs Approved in 2015
Darzalex (daratumumab); Janssen Biotech; For the treatment of multiple myeloma, Approved November 2015.
Darzalex (daratumumab) is a human CD38-directed monoclonal antibody.
Darzalex is specifically indicated for the treatment of patients with multiple myeloma who have received at least three prior lines of therapy including a proteasome inhibitor (PI) and an immunomodulatory agent or who are double-refractory to a PI and an immunomodulatory agent.
Darzalex is supplied as a solution for intravenous infusion. The recommended dose of Darzalex is 16 mg/kg body weight administered as an intravenous infusion according to the following dosing schedule:
Schedule: Weekly – Weeks 1 to 8
Schedule: Every two weeks – Weeks 9 to 24
Schedule: Every four weeks – Week 25 onwards until disease progression.
If a planned dose of Darzalex is missed, administer the dose as soon as possible and adjust the dosing schedule accordingly, maintaining the treatment interval. Read more
Farydak (panobinostat); Novartis; For the treatment of multiple myeloma, Approved February 2015.
Farydak (panobinostat) is a histone deacetylase inhibitor.
Farydak is specifically indicated for use in combination with bortezomib and dexamethasone for the treatment of patients with multiple myeloma who have received at least 2 prior regimens, including bortezomib and an immunomodulatory agent. This indication is approved under accelerated approval based on progression-free survival. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Farydak is supplied as a capsule for oral administration. The recommended dose is 20 mg, taken orally once every other day for three doses per week (on Days 1, 3, 5, 8, 10, and 12) of Weeks 1 and 2 of each 21-day cycle for 8 cycles. Read more
 Natpara (parathyroid hormone); NPS Pharmaceuticals; For the control of hypocalcemia in patients with hypoparathyroidism, Approved January 2015.
Natpara (parathyroid hormone); NPS Pharmaceuticals; For the control of hypocalcemia in patients with hypoparathyroidism, Approved January 2015.
Natpara is a parathyroid hormone. Parathyroid hormone raises serum calcium which releases calcium into the circulation.
Natpara is specifically indicated as an adjunct to calcium and vitamin D to control hypocalcemia in patients with hypoparathyroidism. Because of the potential risk of osteosarcoma, Natpara is recommended only for patients who cannot be well-controlled on calcium supplements and active forms of vitamin D alone.
Natpara is supplied as a solution for subcutaneous injection. The dose of Natpara should be individualized based on total serum calcium (albumin-corrected) and 24-hour urinary calcium excretion. The recommended Natpara dose is the minimum dose required to prevent both hypocalcemia and hypercalciuria. This dose will generally be the dose that maintains total serum calcium (albumin-corrected) within the lower half of the normal range (i.e., between 8 and 9 mg/dL) without the need for active forms of vitamin D and with calcium supplementation sufficient and individualized to meet the patient’s daily requirements. For specific dose adjustments, please see the drug label. Read more
Nuwiq (recombinant Factor VIII); Octapharma; For the prophylaxis and treatment of hemophilia A, Approved September 2015.
Nuwiq Antihemophilic Factor (Recombinant) is an intravenous therapy. The B-domain deleted recombinant Factor VIII (FVIII) is derived from a human cell-line, not chemically modified or fused with another protein.
Nuwiq is specifically indicated for the treatment and prophylaxis of bleeding in pediatric and adult patients with hemophilia A (congenital factor VIII deficiency).
Nuwiq is supplied as a solution for intravenous administration. Please see drug label for dosing specifications. Read more
Praxbind (idarucizumab); Boehringer Ingelheim; For the reversal of the anticoagulant effects of dabigatran, Approved October 2015.
Praxbind (idarucizumab) is a humanized monoclonal antibody fragment (Fab) derived from an IgG1 isotype molecule, whose target is the direct thrombin inhibitor dabigatran.
Praxbind is specifically indicated in patients treated with Pradaxa when reversal of the anticoagulant effects of dabigatran is needed: For emergency surgery/urgent procedures and /or in life-threatening or uncontrolled bleeding.
Praxbind is supplied as a solution for intravenous injection. The recommended dose is 5 g, provided as two separate vials each containing 2.5 g/50 mL idarucizumab. There is limited data to support the administration of an additional 5 g of Praxbind. Read more
Veltassa (patiromer); Relypsa; For the treatment of hyperkalemia, Approved October 2015.
Veltassa (patiromer) is a potassium binder.
Veltassa is specifically indicated for the treatment of hyperkalemia. Veltassa should not be used as an emergency treatment for life-threatening hyperkalemia because of its delayed onset of action.
Veltassa is supplied as a suspension for oral administration. The recommended starting dose of Veltassa is 8.4 grams patiromer once daily. Monitor serum potassium and adjust the dose of Veltassa based on the serum potassium level and the desired target range. The dose may be increased or decreased, as necessary, to reach the desired serum potassium concentration, up to a maximum dose of 25.2 grams once daily. The dose can be up-titrated based on serum potassium level at 1-week or longer intervals, in increments of 8.4 grams.
Veltassa binds to many orally administered medications, which could decrease their absorption and reduce their effectiveness. Administer other oral medications at least 6 hours before or 6 hours after Veltassa. Choose Veltassa or the other oral medication if adequate dosing separation is not possible. Read more
Drugs Approved in 2014
Beleodaq (belinostat); Spectrum Pharmaceuticals; For the treatment of relapsed or refractory peripheral T-cell lymphoma, Approved July 2014.
Beleodaq (belinostat) is a histone deacetylase inhibitor.
Beleodaq is specifically indicated for the treatment of relapsed or refractory peripheral T-cell lymphoma. This indication is approved under accelerated approval based on tumor response rate and duration of response. An improvement in survival or disease-related symptoms has not been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial.
Beleodaq is supplied as a solution for intravenous infusion. The recommended dosage of Beleodaq is 1,000 mg/m2 administered over 30 minutes by intravenous infusion once daily on Days 1-5 of a 21-day cycle. Cycles can be repeated every 21 days until disease progression or unacceptable toxicity. Please see drug label for Beleodaq dosage modifications for hematologic and non-hematologic toxicities. Read more
Blincyto (blinatumomab); Amgen; For the treatment of Philadelphia chromosome-negative relapsed /refractory B cell precursor acute lymphoblastic leukemia, Approved December 2014.
Blincyto (blinatumomab) is an immunotherapy. It engages the body’s T-cells, a type of white blood cell or lymphocyte, to destroy leukemia cells. The drug acts as a connector between a protein called CD19, which is found on the surface of most B-cell lymphoblasts, and CD3, a protein on T-cell lymphocytes.
Blincyto is specifically indicated for the treatment of Philadelphia chromosome-negative relapsed or refractory B-cell precursor acute lymphoblastic leukemia.
Blincyto is supplied as a solution for intravenous infusion. Hospitalization is recommended for the first 9 days of the first cycle and the first 2 days of the second cycle. For all subsequent cycle starts and reinitiation (eg, if treatment is interrupted for 4 or more hours), supervision by a healthcare professional or hospitalization is recommended. Do not flush the Blincyto infusion line, especially when changing infusion bags. Flushing when changing bags or at completion of infusion can result in excess dosage and complications. The recommended dosing schedule is as follows:
A single cycle of treatment of Blincyto consists of 4 weeks of continuous intravenous infusion followed by a 2-week treatment-free interval.
• For patients at least 45 kg in weight:
– In Cycle 1, administer Blincyto at 9 mcg/day on Days 1–7 and at 28 mcg/day on Days 8–28.
– For subsequent cycles, administer Blincyto at 28 mcg/day on Days 1–28.
• Allow for at least 2 weeks treatment-free between cycles of Blincyto.
• A treatment course consists of up to 2 cycles of Blincyto for induction followed by 3 additional cycles for consolidation treatment (up to a total of 5 cycles). Read more
Imbruvica (ibrutinib); Pharmacyclics; For the treatment of chronic lymphocytic leukemia and Waldenstrom macroglobulinemia, Approved February 2014.
Imbruvica (ibrutinib) is an orally available, selective inhibitor of Bruton’s tyrosine kinase (Btk), a gene that is disrupted in the human disease X-linked agammaglobulinemia (XLA). BTK is a signaling molecule of the B-cell antigen receptor (BCR) and cytokine receptor pathways.
Imbruvica is specifically approved for chronic lymphocytic leukemia in patients who have received at least one prior therapy.
Imbruvica is supplied as a capsule for oral administration. The recommended dose is 420 mg taken orally once daily (three 140 mg capsules once daily). Capsules should be taken orally with a glass of water. Do not open, break, or chew the capsules. Read more
Sylvant (siltuximab); Janssen Biotech; For the treatment of multicentric Castleman’s disease, Approved April 2014.
Sylvant (siltuximab) is an anti-interleukin-6 (IL-6) chimeric monoclonal antibody that binds to human IL-6. IL-6 is a multifunctional cytokine produced by various cells such as T cells, B cells, monocytes, fibroblasts, and endothelial cells. Dysregulated overproduction of IL-6 from activated B cells in affected lymph nodes has been implicated in the pathogenesis of, or mechanism causing, multicentric Castleman’s disease.
Sylvant is specifically indicated for the treatment of patients with multicentric Castleman’s disease who are human immunodeficiency virus (HIV) negative and human herpesvirus-8 (HHV-8) negative.
Sylvant is supplied as a solution for intravenous infusion. The recommended dose is 11 mg/kg given over 1 hour as an intravenous infusion administered every three weeks until treatment failure. Read more
Zydelig (idelalisib); Gilead; For the treatment of relapsed CLL, follicular B-cell NHL and small lymphocytic lymphoma, Approved July 2014.
Zydelig (idelalisib) is a small molecule inhibitor of phosphoinositide-3 kinase (PI3K) delta, an intracellular signaling component. PI3K-delta is expressed primarily in blood-cell lineages, including cells that cause or mediate hematologic malignancies.
Zydelig is specifically indicated for the following:
- Relapsed chronic lymphocytic leukemia in combination with rituximab, in patients for whom rituximab alone would be considered appropriate therapy due to other co-morbidities.
- Relapsed follicular B-cell non-Hodgkin lymphoma in patients who have received at least two prior systemic therapies.
- Relapsed small lymphocytic lymphoma in patients who have received at least two prior systemic therapies.
Zydelig is supplied as a tablet for oral administration. The recommended maximum starting dose of Zydelig is 150 mg administered orally twice daily. Zydelig can be taken with or without food. Tablets should be swallowed whole. Continue treatment until disease progression or unacceptable toxicity. Read more
Drugs Approved in 2013
Gazyva (obinutuzumab); Genentech; For the treatment of previously untreated chronic lymphocytic leukemia, Approved October of 2013.
Gazyva (obinutuzumab) is a humanized anti-CD20 monoclonal antibody of the IgG1 subclass. It recognizes a specific epitope of the CD20 molecule found on B-cells.
Gazyva is specifically indicated for use in combination with chlorambucil for the treatment of patients with previously untreated chronic lymphocytic leukemia.
Gazyva is supplied as a solution for intravenous administration. The dose of Gazyva is 1000 mg, administered intravenously, with the exception of the first infusions in cycle 1, which are administered on day 1 (100 mg) and day 2 (900 mg). Gazyva is administered in six cycles, each consisting of 28 days. Read more
Pomalyst (pomalidomide); Celgene; For the treatment of relapsed and refractory multiple myeloma, Approved February 2013.
Pomalyst (pomalidomide) is an immunomodulatory antineoplastic agent. It inhibits proliferation and induces apoptosis of hematopoietic tumor cells, enhances T cell- and natural killer cell-mediated immunity and inhibits production of pro-inflammatory cytokines by monocytes.
Pomalyst is specifically indicated for patients with multiple myeloma who have received at least two prior therapies including lenalidomide and bortezomib and have demonstrated disease progression on or within 60 days of completion of the last therapy.
Pomalyst is supplied as a capsule for oral administration. The recommended starting dose is 4 mg once daily orally on Days 1-21 of repeated 28-day cycles until disease progression. It should be taken without food (at least 2 hours before or 2 hours after a meal). Pomalyst may be given in combination with dexamethasone. Read more
Revlimid (lenalidomide); Celgene; For the treatment of mantle cell lymphoma, Approved June 2013.
Revlimid (lenalidomide), a thalidomide analogue, is an immunomodulatory agent with antiangiogenic and antineoplastic properties.
Revlimid is specifically indicated for the treatment of patients with mantle cell lymphoma (MCL) whose disease has relapsed or progressed after two prior therapies, one of which included bortezomib.
The recommended dose in this population is 25 mg/day orally on Days 1-21 of repeated 28-day cycles for relapsed or refractory mantle cell lymphoma. Treatment should be continued until disease progression or unacceptable toxicity. Read more
Valchlor (mechlorethamine) gel; Ceptaris Therapeutics; For the treatment of Stage IA/IB mycosis fungoides-type cutaneous T-cell lymphoma, Approved August 2013.
Valchlor is a gel formulation of mechlorethamine, an alkylating agent which inhibits rapidly proliferating cells.
Valchlor is specifically indicated for the topical treatment of Stage IA and IB mycosis fungoids-type cutaneous T-cell lymphoma in patients who have received prior skin-directed therapy.
Valchlor is supplied as a gel for topical administration. The recommendation is to apply a thin film of Valchlor gel once daily to affected areas of the skin. Upon improvement, treatment with Valchlor can be restarted at a reduced frequency of once every 3 days. If reintroduction of treatment is tolerated for at least one week, the frequency of application can be increased to every other day for at least one week and then to once daily application if tolerated. Read more
Drugs Approved in 2012
Bosulif (bosutinib); Pfizer; For the treatment of Ph+ chronic myelogenous leukemia, Approved September 2012.
Bosulif (bosutinib) is a tyrosine kinase inhibitor. Tyrosine kinases a subclass of protein kinase. Tyrosine kinases function as an on or off switch in many cellular functions. They can become mutated and cause unregulated growth of the cell, which is a necessary step for the development of cancer. Bosutinib inhibits the Bcr-Abl kinase that promotes CML and also inhibits the Src-family kinases.
Bosulif is specifically indicated for the treatment of adults with chronic, accelerated, or blast phase Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia with resistance or intolerance to prior therapy.
Bosulif is supplied as a tablet for oral administration. The recommended dose is 500 mg orally once daily with food. Continue treatment until disease progression or patient intolerance. Read more
Iclusig (ponatinib); Ariad Pharmaceuticals; For the treatment of chronic myeloid leukemia and Philadelphia chromosome-positive acute lymphoblastic leukemia, Approved December 2012.
Iclusig (ponatinib) is a small-molecule dual Abl/Src protein inhibitor.
Iclusig is specifically indicated for the treatment of adult patients with chronic phase, accelerated phase, or blast phase chronic myeloid leukemia (CML) that is resistant or intolerant to prior tyrosine kinase inhibitor therapy or Philadelphia chromosome positive acute lymphoblastic leukemia (Ph+ALL) that is resistant or intolerant to prior tyrosine kinase inhibitor therapy.
Iclusig is supplied as a tablet for oral administration. The recommended initial dose is 45 mg administered orally once daily. Treatment should be continued until evidence of disease progression or unacceptable toxicity. Dose modifications should be considered for myelosuppression, non-hematologic adverse reactions, and use with strong CYP3A inhibitors. See the drug label for appropriate dose modifications. Read more
Kyprolis (carfilzomib); Onyx Pharmaceuticals; For the treatment of multiple myeloma, Approved July 2012.
Kyprolis (carfilzomib) is a proteasome inhibitor. Carfilzomib had antiproliferative and proapoptotic activities in vitro in solid and hematologic tumor cells. In animals, carfilzomib inhibited proteasome activity in blood and tissue and delayed tumor growth.
Kyprolis is specifically indicated for the treatment of multiple myeloma in patients who have received at least two prior therapies including bortezomib and an immunomodulatory agent and have demonstrated disease progression on or within 60 days of completion of the last therapy.
Kyprolis is supplied as a solution for intravenous administration. Kyprolis should be administered intravenously over 2 to 10 minutes, on two consecutive days, each week for three weeks followed by a 12-day rest period. Each 28-day period is considered one treatment cycle. In Cycle 1, Kyprolis should be administered at a dose of 20 mg/m2. If tolerated in Cycle 1, the dose should be escalated to 27 mg/m2 beginning in Cycle 2 and continued at 27 mg/m2 in subsequent cycles. Treatment may be continued until disease progression or until unacceptable toxicity occurs. Read more
Marqibo (vinCRIStine sulfate LIPOSOME injection); Talon Therapeutics; For the treatment of Ph- acute lymphoblastic leukemia, Approved August 2012.
Marqibo (vinCRIStine sulfate LIPOSOME injection) is vincristine encapsulated in sphingomyelin/cholesterol liposomes. The encapsulation formulation was designed to enhance efficacy, with the potential for reduced toxicity. Vincristine is a vinca alkaloid; it is thought to work by interfering with cancer cell growth during mitosis.
Marqibo is specifically indicated for the treatment of adults with Philadelphia chromosome-negative (Ph-) acute lymphoblastic leukemia in second or greater relapse or whose disease has progressed following two or more anti-leukemia therapies.
Marqibo is supplied as a solution for intravenous injection. The recommended initial dose is 2.25 mg/m2 intravenously over one hour once every seven days. Read more
Neutroval (tbo-filgrastim); Teva Pharmaceutical; For the reduction in the duration of severe chemotherapy-induced neutropenia, Approved August 2012.
Neutroval (tbo-filgrastim) is a human granulocyte colony-stimulating factor (G-CSF) produced by recombinant DNA technology. Tbo-filgrastim binds to G-CSF receptors and stimulates proliferation of neutrophils. G-CSF is known to stimulate differentiation commitment and some end-cell functional activation, which increases neutrophil counts and activity.
tbo-filgrastim is specifically approved to reduce the duration of severe neutropenia in patients with non-myeloid malignancies receiving myelosuppressive anti-cancer drugs associated with a clinically significant incidence of febrile neutropenia.
tbo-filgrastim is supplied as a solution for subcutaneous injection. The recommended dose of tbo-filgrastim is 5 mcg/kg per day administered as a subcutaneous injection. Administer the first dose of tbo-filgrastim no earlier than 24 hours following myelosuppressive chemotherapy. Do not administer tbo-filgrastim within 24 hours prior to chemotherapy. Read more
Omontys (peginesatide); Affymax; For the treatment of anemia due to chronic kidney disease, Approved March 2012.
Omontys (peginesatide) is a peptide-based erythropoiesis stimulating agent (ESA). Peginesatide binds to and activates the human erythropoietin receptor and stimulates erythropoiesis in human red cell precursors.
Omontys is specifically indicated for the treatment of anemia due to chronic kidney disease in adult patients on dialysis.
Omontys is supplied as a solution for subcutaneous or intravenous injection. The recommended initial dose is 0.04 mg/kg body weight administered as a single intravenous or subcutaneous injection once monthly. In patients previously receiving epoetin alfa or darbepoetin alfa, the recommended starting monthly dose of Omontys should be estimated on the basis of the weekly dose of epoetin alfa or darbepoetin alfa at the time of substitution. See label for specific dosing levels. Read more
Synribo (omacetaxine mepesuccinate); Teva Pharmaceutical; For the treatment of chronic or accelerated phase chronic myeloid leukemia, Approved October 2012.
Synribo (omacetaxine mepesuccinate) is a cephalotaxine ester. It is a protein synthesis inhibitor and is independent of direct Bcr-Abl binding.
Synribo is specifically approved for the treatment of adults with chronic or accelerated phase chronic myeloid leukemia with resistance and/or intolerance to two or more tyrosine kinase inhibitors.
Synribo is supplied as a solution for subcutaneous administration. The recommended initial dose of the drug is as follows: Induction Schedule: 1.25 mg/m2 administered subcutaneously twice daily for 14 consecutive days every 28 days, over a 28-day cycle. Cycles should be repeated every 28 days until patients achieve a hematologic response. Maintenance Dosing: 1.25 mg/m2 administered subcutaneously twice daily for 7 consecutive days every 28 days, over a 28-day cycle. Treatment should continue as long as patients are clinically benefiting from therapy. Read more
Drugs Approved in 2011
Adcetris (brentuximab vedotin); Seattle Genetics; For the treatment of Hodgkin lymphoma and anaplastic large cell lymphoma, Approved August 2011.
Adcetris (brentuximab vedotin) is an antibody-drug conjugate comprised of an anti-CD30 antibody joined by an enzyme cleavable linker to a potent, synthetic drug payload, monomethyl auristatin E (MMAE), using Seattle Genetics’ proprietary technology. Brentuximab vedotin is designed to be stable in the bloodstream, but to release MMAE upon internalization into CD30-expressing tumor cells, resulting in a targeted cell-killing effect.
Adcetris is specifically approved for 1) Hodgkin lymphoma after failure of autologous stem cell transplant (ASCT) or after failure of at least two prior multi-agent chemotherapy regimens in patients who are not ASCT candidates and 2) systemic anaplastic large cell lymphoma after failure of at least one prior multi-agent chemotherapy regimen.
Adcetris is supplied as a solution for intravenous infusion. The recommended dose is 1.8 mg/kg administered only as an intravenous infusion over 30 minutes every three weeks. Read more
Erwinaze (asparaginase Erwinia chrysanthemi); Eusa Pharma; For the treatment of acute lymphoblastic leukemia, Approved November of 2011.
Erwinaze (asparaginase Erwinia chrysanthemi) contains an asparaginase specific enzyme derived from Erwinia chrysanthemi. The mechanism of action of Erwinaze thought to be based on the inability of leukemic cells to synthesize asparagine due to lack of asparagine synthetase activity, resulting in cytotoxicity specific for leukemic cells.
Erwinaze is specifically approved as a component of a multi-agent chemotherapeutic regimen for the treatment of patients with acute lymphoblastic leukemia who have developed hypersensitivity to E. coli-derived asparaginase.
Erwinaze is supplied as a solution for intramuscular administration. The recommended initial dose of the drug is as follows:
To substitute for a dose of pegaspargase: 25,000 International Units/m2 administered intramuscularly three times a week (Monday/Wednesday/Friday) for six doses for each planned dose of pegaspargase.
To substitute for a dose of native E. coli asparaginase: 25,000 International Units/m2 administered intramuscularly for each scheduled dose of native E. coli asparaginase within a treatment. Read more
Ferriprox (deferiprone); Apotex; For the treatment of transfusional iron overload due to thalassemia, Approved October 2011.
Ferriprox (deferiprone) is a chelating agent with an affinity for ferric ion (iron III). Deferiprone binds with ferric ions to form neutral complexes that are stable over a wide range of pH values.
Ferriprox is specifically indicated for patients with transfusional iron overload due to thalassemia syndromes when current chelation therapy is inadequate.
Ferriprox is supplied as a tablet for oral administration. The recommended initial dose is 25 mg/kg, orally, three times per day for a total of 75 mg/kg/day. The maximum dose is 33 mg/kg, three times per day for a total of 99 mg/kg/day. Read more
Jakafi (ruxolitinib); Incyte; For the treatment of myelofibrosis, Approved November 2011.
Jakafi (ruxolitinib) is a kinase inhibitor and inhibits Janus Associated Kinases (JAKs) JAK1 and JAK2, which mediate the signaling of a number of cytokines and growth factors that are important for hematopoiesis and immune function. Myelofibrosis is a myeloproliferative neoplasm known to be associated with dysregulated JAK1 and JAK2 signaling.
Jakafi is specifically approved for intermediate or high-risk myelofibrosis, including primary myelofibrosis, post-polycythemia vera myelofibrosis, and post-essential thrombocythemia myelofibrosis.
Jakafi is supplied as a tablet for oral administration. The recommended initial dose is based on platelet count. A complete blood count (CBC) and platelet count must be performed before initiating therapy, every 2 to 4 weeks until doses are stabilized, and then as clinically indicated. The proposed starting doses are as follows:
Platelet Count greater than 200 X 10(9)/L – Starting Dose 20 mg orally twice daily.
Platelet Count 100 X 10(9)/L to 200 X 10(9)/L – Starting Dose 15 mg orally twice daily. Read more
Xarelto (rivaroxaban); Bayer; For the prophylaxis of deep vein thrombosis during knee or hip replacement surgery, Approved July 2011.
Xarelto (rivaroxaban) is a factor Xa inhibitor that selectively blocks the active site of factor Xa and does not require a cofactor (such as Anti-thrombin III) for activity. Activation of factor X to factor Xa (FXa) via the intrinsic and extrinsic pathways plays a central role in the cascade of blood coagulation.
Xarelto is specifically indicated for the prophylaxis of deep vein thrombosis, which may lead to pulmonary embolism in patients undergoing knee or hip replacement surgery.
Xarelto is supplied as a tablet for oral administration. The recommended initial dose is 10 mg taken orally once daily with or without food. The initial dose should be taken at least 6 to 10 hours after surgery once hemostasis has been established. For hip replacement surgery a treatment duration of 35 days is recommended. For knee replacement surgery a treatment duration of 12 days is recommended. Read more
Drugs Approved in 2010
Vpriv (velaglucerase alfa for injection); Shire Pharmaceuticals; For the treatment of type 1 Gaucher disease, Approved March 2010.
Vpriv (velaglucerase alfa) is a human glucocerebrosidase product developed using the company’s proprietary gene activation technology. Gaucher disease, caused by a deficiency of the enzyme glucocerebrosidase, results in the accumulation of a toxic glycolipid substrate, called glucocerebroside. Velaglucerase alfa supplements replace beta-glucocerebrosidase, the enzyme that catalyzes the hydrolysis of glucocerebroside, reducing the amount of accumulated glucocerebroside and correcting the pathophysiology of Gaucher disease.
Vpriv is specifically indicated for long-term enzyme replacement therapy for pediatric and adult patients with type 1 Gaucher disease.
Vpriv is supplied as a lyophilized powder which requires reconstitution and is intended for intravenous infusion. The recommended dose is 60 Units/kg administered every other week as a 60-minute intravenous infusion. Read more
References:
FDA Approved Drugs in Hematology | CenterWatch https://www.centerwatch.com/drug-information/fda-approved-drugs/therapeutic-area/6/hematology#.WzauJO7jvLY
New Drugs in Hematology http://www.mdpi.com/journal/pharmaceuticals/special_issues/Hematology