Pure Red Cell Aplasia
Background:
Pure red cell aplasia (PRCA) is an uncommon disorder in which maturation arrest occurs in the formation of erythrocytes.
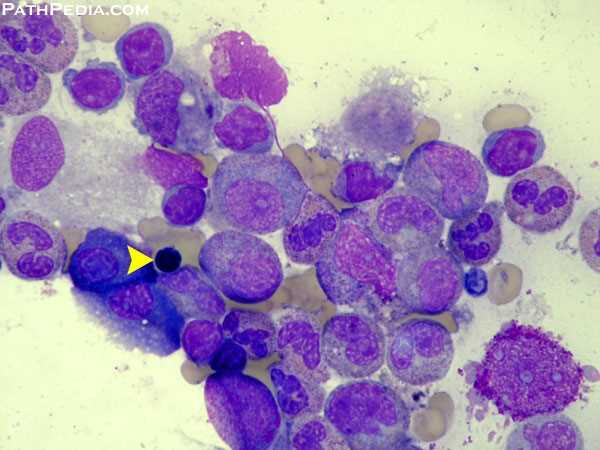
Erythroblasts are virtually absent in bone marrow; however, WBC and platelet production is normal.
The anemia due to PRCA is usually normocytic but can be macrocytic.
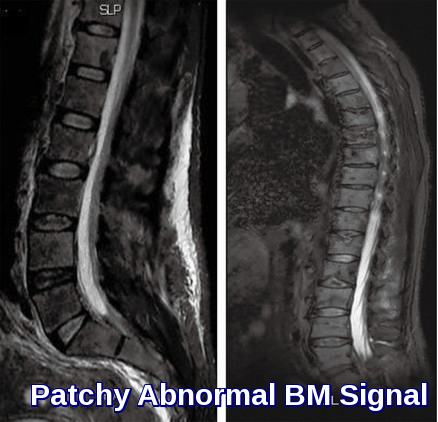
The characteristics of PRCA include severe anemia, a reticulocyte count <1%, and the presence of <0.5% mature erythroblasts in the bone marrow. The bone marrow is usually normocellular.
PRCA can be transient and reversible.
Transient erythroblastopenia of childhood (TEC) can occur after viral infections.
PRCA due to medications and infections are often reversible.
Classification of PRCA:
Acute:
- This is usually a self-limiting episode in patients with congenital hemolytic anemia.
- It is due to a parvovirus infection (Fifth’s disease).
Chronic:
Congenital (Diamond Blackfan Syndrome):
Usually inherited but mode uncertain.
Often associated with other minor congenital abnormalities.
Anemia usually begins in the first few days of life but may be delayed for several years.
Very few normoblasts are seen in the bone marrow.
The HbF is usually raised.
Many patients respond to steroids and others require long-term supportive blood transfusions.
Acquired:
In adults, most cases of chronic PRCA are idiopathic.
Secondary PRCA occurs in patients with conditions such as autoimmune disorders, thymomas, systemic lupus erythematosus, hematologic malignancies, and solid tumors.
Treatment and Prognosis:
- The initial treatment plan should include transfusions for patients who are severely anemic.
- Anemia is more severe in patients with pure red cell aplasia (PRCA) who have ongoing hemolysis (aplastic crises).
- Medications that could cause PRCA should be discontinued.
- Children with PRCA should be observed and not aggressively treated to avoid corticosteroid-related growth retardation. This caution is feasible since PRCA in children is often transient and reversible. However, transfusion should be administered if indicated.
- Infections should be treated. High-dose intravenous immunoglobin therapy (IVIG) should be considered for parvovirus B19 infections.
- PRCA due to medication or infections is usually reversible within a few months, if not earlier. However, immunotherapy may be needed to reverse erythropoiesis-stimulating agent (Erythropoietin)–related PRCA.
- Underlying conditions should be treated. These conditions include a thymoma, hematological malignancies such as T-cell large granular lymphocyte leukemia, solid tumors, and systemic lupus erythematosus (SLE). Surgery or gamma irradiation of the thymus should be considered in a patient with thymoma.
- PRCA considered to be idiopathic and due to autoimmunity should be initially treated with corticosteroids. A response is expected within 4-6 weeks in about 45% of patients. Corticosteroids should be judiciously given to children to avoid growth retardation.
- Immunosuppressive agents have an important role. Immunosuppressive agents used in PRCA include cyclophosphamide, 6-mercaptopurine, azathioprine, and cyclosporine A. Rituximab has been reported to be effective in managing PRCA. Antithymic globulin (ATG) is another therapeutic option. Danazol has been helpful in some cases but is contraindicated in children. Plasmapheresis has been used to remove autoantibodies.
- Autologous and nonmyeloablative allogeneic peripheral stem cell transplantation have been used, especially in patients refractory to therapy.
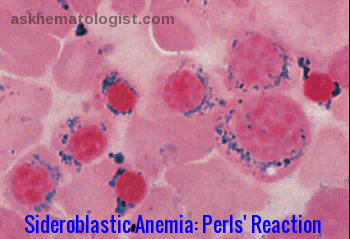
- Iron chelation should be considered in patients who have had multiple transfusions and have evidence of iron overload e.g. with deferasirox (Exjade).
Summary:
Pure red cell aplasia (PRCA) is a syndrome defined by normocytic normochromic anemia with severe reticulocytopenia and marked reduction or absence of erythroid precursors from the bone marrow. Diamond-Blackfan anemia is a congenital form of PRCA. Acquired PRCA may be either a primary disorder or secondary to some other disorder or agent. Primary acquired PRCA is an autoimmune disorder that is frequently antibody-mediated. Myelodysplastic syndromes may also present with the morphologic appearance of PRCA. Secondary acquired PRCA may be associated with collagen vascular/autoimmune disorders such as systemic lupus erythematosus; lymphoproliferative disorders such as chronic lymphocytic leukemia or large granular lymphocyte leukemia; infections, particularly B19 parvovirus; thymoma and other solid tumors; or a variety of other disorders, drugs, or toxic agents. The therapeutic approach to PRCA typically involves immunosuppression, but specific pathogenic subtypes are associated with specific therapeutic approaches. Cyclosporine A, with or without concurrent corticosteroids, appears to be the single most effective immunosuppressive agent.
References:
Robert T. Means Jr. Pure red cell aplasia http://www.bloodjournal.org/content/128/21/2504
Paul Schick, MD; Emmanuel C Besa, MD. Pure Red Cell Aplasia: Practice Essentials, Pathophysiology, Etiology http://emedicine.medscape.com/article/205695-overview
Hoffman R, Benz EJ, Silberstein LE, Heslop H, Weitz J, Anastasi J. Biology of Erythropoiesis, Erythroid Differentiation, and Maturation. Hematology: Basic Principles and Practice. 6th ed. Philadelphia, PA: Churchill Livingstone; 2013.
Young NS. Pure Red Cell Aplasia. In: Kaushansky K, Lichtman MA, Prchal JT, Levi MM, Press OW, Burns LJ, Caligiuri MA, eds. Williams Hematology. 9th ed. New York, NY: McGraw-Hill Education; 2016. 539-48.
Herbert KE, Prince HM, Westerman DA. Pure red-cell aplasia due to parvovirus B19 infection in a patient treated with alemtuzumab. Blood. 2003. 101:1654.







May i have any contact information for appointment with the doctor. I have a 3-4 year old nephew who is right now suffering with the Pure Red Cell Aplasia.
Hi Jawad,
Thank you for your comment.
I would suggest sending me his CBC and any other previous investigations including bone marrow in a private message through our “contact us” form or our email [email protected] to have a look and advise.
Regards,