Miscellaneous Red Cell Abnormalities
Introduction
In the chapter of Miscellaneous Red Cell Abnormalities, we will discuss some of the commonly seen red blood cell abnormalities.
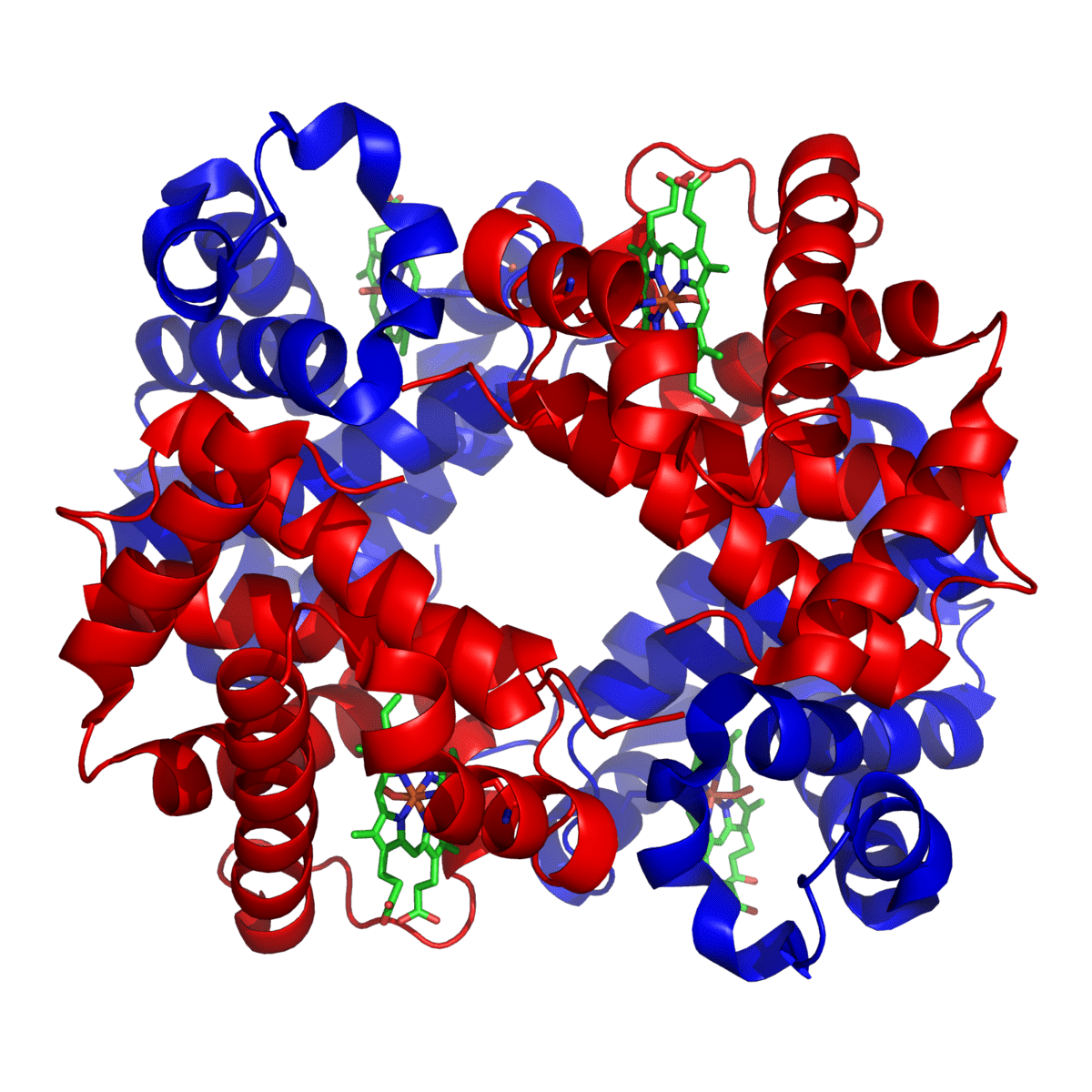
Adult human bone marrow synthesizes 4 X 1014 molecules of hemoglobin every second. Heme and globin chains (alpha and beta) in adults are manufactured in separate cell compartments—mitochondria and cytoplasm, respectively—and then combined in the cytoplasm in an amazingly accurate manner. Four major problems can manifest during this delicate process:
- Qualitative defects of globin chain synthesis result in hemoglobinopathies such as sickle cell disease.
- Quantitative defects of globin chain synthesis result in hemoglobinopathies such as thalassemia.
- Defects in the synthesis of the heme portion result in porphyrias.
- Defects involving incorporation of iron into the heme molecule result in sideroblastic anemias.
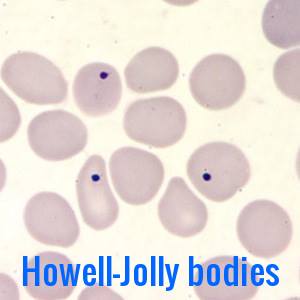
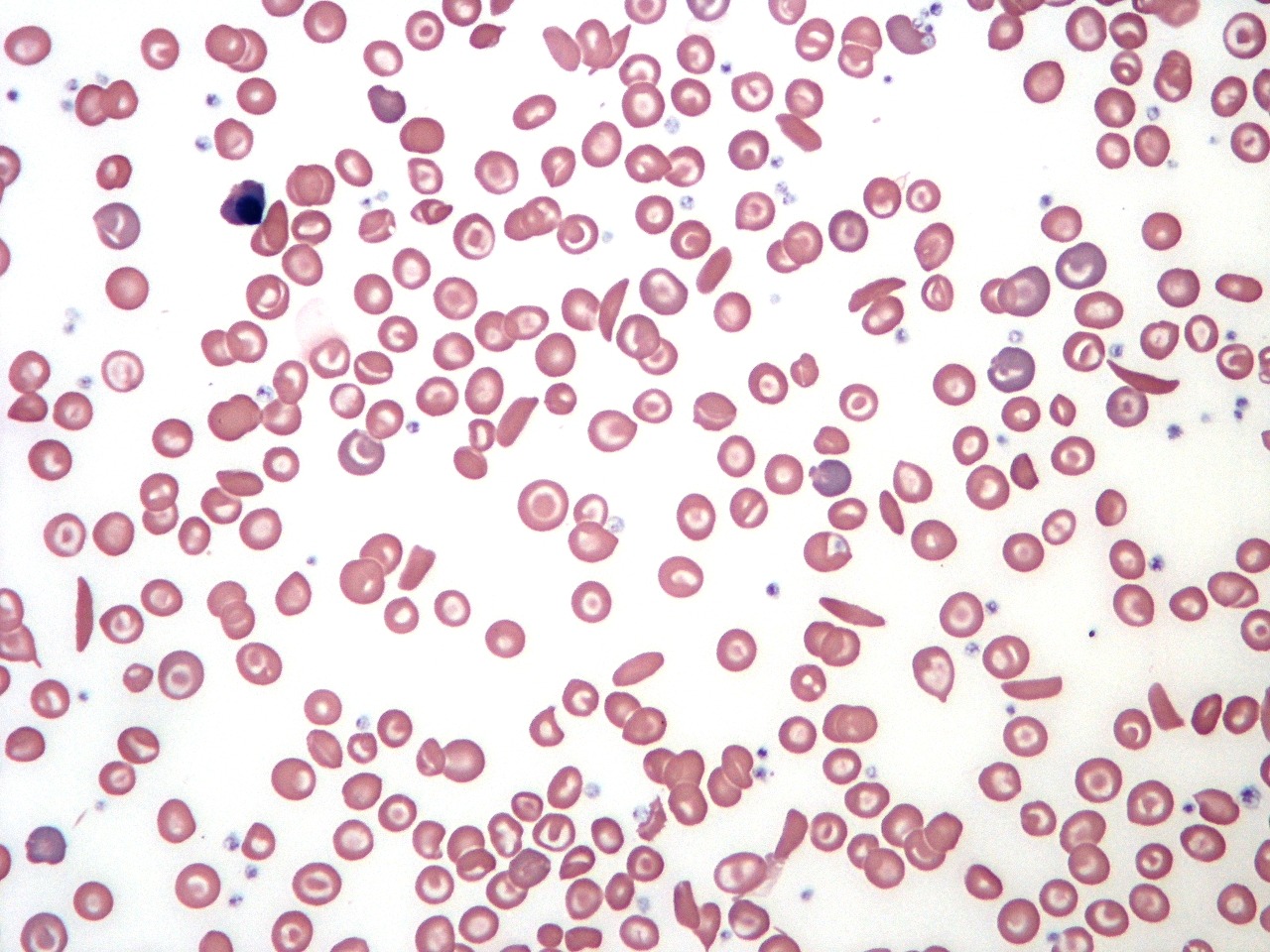
Howell-Jolly bodies
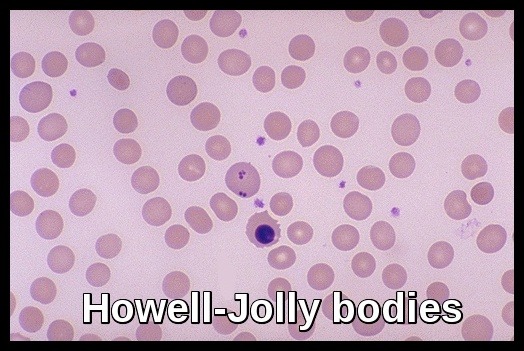
The RBC in the center of the field contains several Howell-Jolly bodies or inclusions of nuclear chromatin remnants. There is also a nucleated RBC just beneath this RBC. Abnormal and aged RBC’s are typically removed by the spleen. The appearance of increased poikilocytosis, anisocytosis, and RBC inclusions suggest that a spleen is not present.
Howell-Jolly bodies are nuclear remnants found in red blood cells (erythrocytes) under various pathological states. They most commonly present in patients with absent or impaired function of the spleen; this is because one of the spleen’s functions is to filter deranged blood cells and remove the intracellular inclusions left by the erythrocyte precursors. William Howell and Justin Jolly in the early 1900s first discovered them in the early 1900s.
Howell-Jolly bodies occur predominantly following splenectomy and in hyposplenic conditions such as coeliac disease. Post-splenectomy blood films show also the following features: target cells, acanthocytes, spherocytes, nucleated red cells, Pappenheimer bodies, and Heinz bodies. The spleen is also responsible for the surface remodeling of red cells.
Following splenectomy, other blood changes including transient leucocytosis and thrombocytosis are commonly seen.
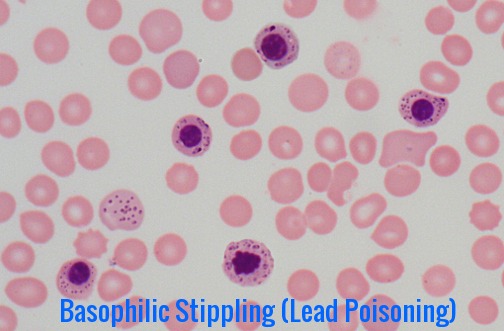
Basophilic Stippling
Basophilic stippling is one example of several clinically significant miscellaneous red cell abnormalities in which erythrocyte inclusions are identified on peripheral blood smears. The presence of basophilic stippling is attributed to aggregates of ribosomes or fragments of ribosomal RNA precipitated throughout the cytoplasm of circulating erythrocytes. This finding is associated with acquired and heritable hematologic disorders affecting erythropoiesis and erythrocyte maturation.
Basophilic stippling is a frequent manifestation of hematologic disease in the peripheral blood, and it is also observable in bone marrow aspirates. It is implicated in cases of lead poisoning but can be an indicator of various heavy metal toxicities. Alternative causes of basophilic stippling such as hemoglobinopathies, nutritional deficiencies, severe infections, sideroblastic anemia, TTP, and myelodysplasia warrant consideration as well in the context of appropriate clinical history.
Congenital Dyserythropoietic Anemias (CDA)
This is a group of rare miscellaneous red cell abnormalities. Congenital dyserythropoietic anemias belong to a group of inherited conditions characterized by a maturation arrest during erythropoiesis with a reduced reticulocyte production.
CDA is characterized by ineffective erythropoiesis with erythroid cell death within the bone marrow.
Megaloblastoid changes may occur and erythroid multinuclearity is typical.
There are at least three varieties of CDA one of which (CDA II) is associated with lysis of the RBCs by acidified group matched allogeneic sera (Ham’s test).
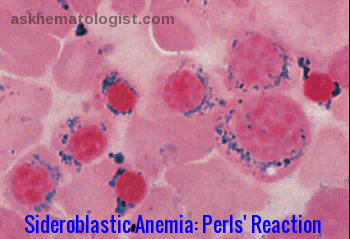
Sideroblastic Anemias
- These are a group of dyserythropoietic disorders in which iron-containing granules (demonstrated by Prussian blue stain – Perls’ reaction) surround the nuclei of some erythroblasts.
- The disorder may be hereditary or acquired.
- The acquired form may be secondary to certain drugs (e.g. antituberculous agents like isoniazid), lead poisoning, other toxic conditions, nutritional deficiencies (copper, vitamin B6), alcohol, as a clonal disorder (myelodysplasia) which may progress to acute leukemia or idiopathic.
- Treatment of sideroblastic anemia may include removal of toxic agents; administration of pyridoxine, thiamine, or folic acid; transfusion (along with antidotes if iron overload develops from transfusion); other medical measures; or bone marrow or liver transplantation.
Alcohol-induced bone marrow damage
- Excessive alcohol intake can result in dyserythropoiesis as well as morphological changes due to vitamin deficiencies.
- Bone marrow findings took the form of ineffective erythropoiesis associated with impaired iron utilization, vacuolated proerythroblasts, multinuclear erythroblasts, megaloblasts, and iron-containing plasma cells as well as vacuolated precursor cells of the granulocytopoietic series.
- In the differential diagnosis, alcohol-induced bone marrow damage is to be distinguished from the myelodysplastic syndrome of the RA and RARS form.
- Alcohol-induced bone marrow damage is reversible. The toxic defect probably does not reside in the stem cell but is more peripheral.
References:
Jones, Kathy W. “Evaluation of Cell Morphology and Introduction to Platelet and White Blood Cell Morphology.” (2010).https://www.semanticscholar.org/paper/Evaluation-of-Cell-Morphology-and-Introduction-to-Jones/10dffb91283c63e7d275f1af53d980aa84f82620
Sears, MD, Udden, MD. Howell-Jolly Bodies: A Brief Historical Review. The American Journal of the Medical Sciences Volume 343, Issue 5, May 2012, Pages 407–409.
Cheson, B. D; Rom, W. N; Webber, R. C (1984). “Basophilic stippling of red blood cells: A nonspecific finding of multiple etiology”. American Journal of Industrial Medicine. 5 (4): 327–34.
Denecke, Jonas; Marquardt, Thorsten (2009-09-01). “Congenital dyserythropoietic anemia type II (CDAII/HEMPAS): Where are we now?”. Biochimica et Biophysica Acta (BBA) – Molecular Basis of Disease. Genetic Glycosylation Diseases. 1792 (9): 915–920.
McLintock LA, Fitzsimons EJ. Erythroblast iron metabolism in sideroblastic and sideropenic states. Hematology. 2002;7:189-95.
Girard DE, Kumar KL, McAfee JH. Hematologic effects of acute and chronic alcohol abuse. Hematol Oncol Clin North Am 1987; 1:321.
Sanchez JR, Lynch DT. Histology, Basophilic Stippling. [Updated 2020 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545259/
Achille Iolascon, Maria Rosaria Esposito, Roberta Russo. Clinical Aspects And Pathogenesis Of Congenital Dyserythropoietic Anemias: From Morphology To Molecular Approach. http://www.haematologica.org/content/97/12/1786
Keywords:
Red cell abnormalities, red cell anomalies, red cell abnormalities morphology, red cell abnormalities indicative of hemolysis, red cell abnormal shape, red cell defects, why is my rbc morphology abnormal, what causes rbc hemolysis, what does abnormal red blood cells indicate, abnormality of red blood cells, what is red cell morphology, clinical significance of rbc indices, types of red blood cell disorders.







Amazing pictures & information. Thank you for sharing.