Sickle Cell Disease
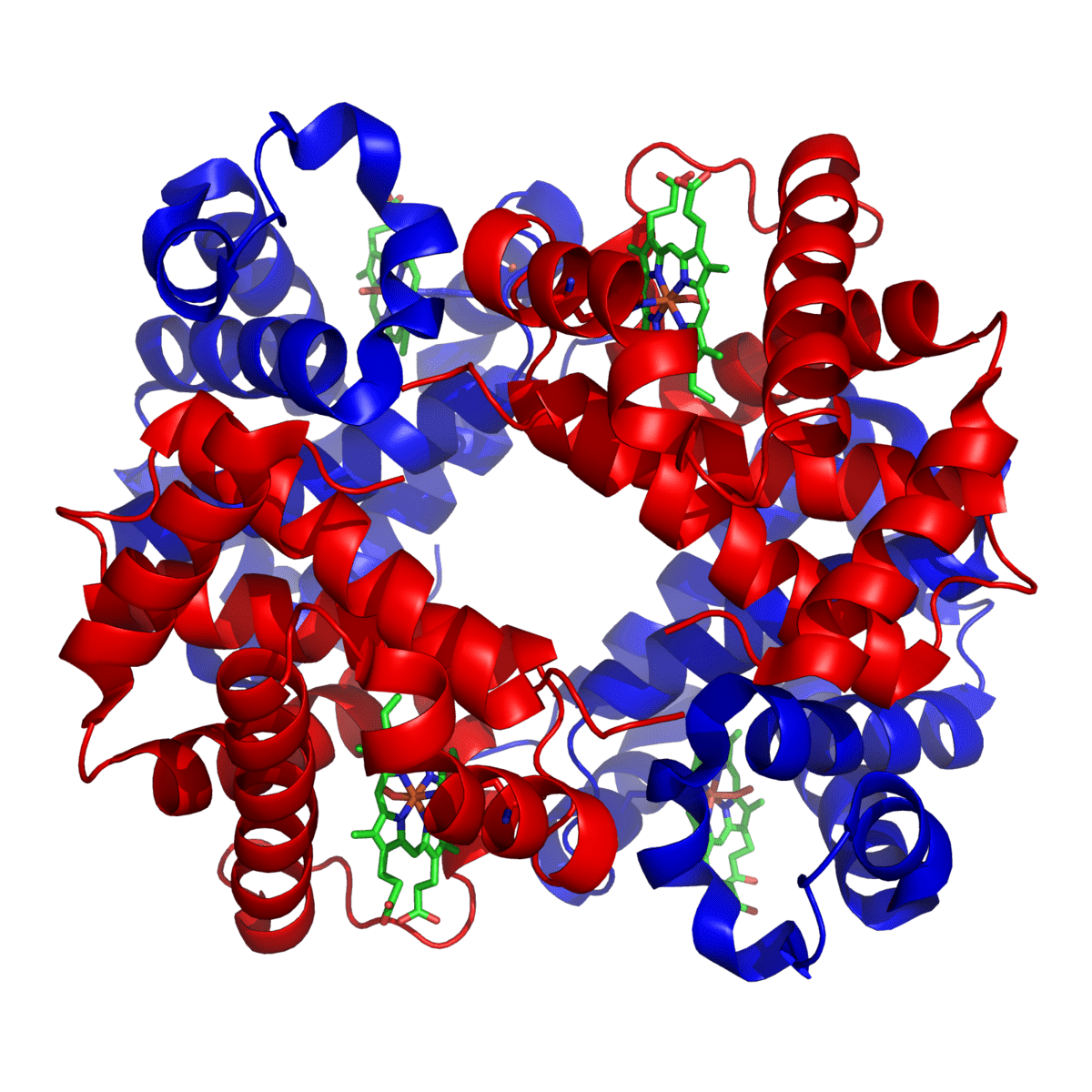
Sickle cell disease (HbS) is a severe hereditary form of anemia in which a mutated form of hemoglobin distorts the red blood cells (RBC’s) into a crescent shape at low oxygen levels.
Sickle cell disease (HbS) is commonest among those of African descent.
In this disease, a single base mutation in the β-globin gene leads to the substitution of valine for glutamine at the 6th amino acid position of the β-globin chain. High levels of deoxygenated sickle Hb form reversible fibrils leading to sickling of the red cells.
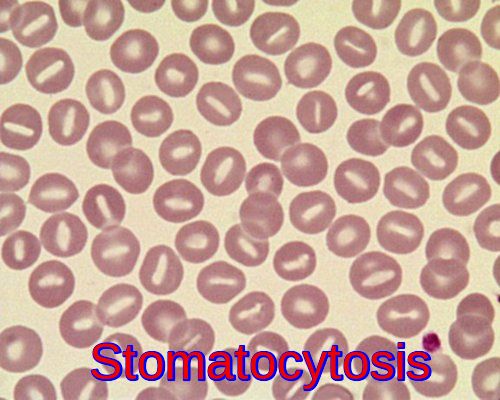
The abnormal Hb SS is prone to form tactoids with crystallization in the RBC’s when oxygen tension is low, and the RBC’s change shape to long, thin sickle cells that are “sticky” and sludge in capillaries, further decreasing blood flow and oxygen tension. The sickled RBCs tend to adhere to endothelium, and the bioavailability of endothelial nitric oxide is reduced as well, further promoting vaso-occlusion.
Clinical features:
The heterozygous state (Sickle Cell Trait – HbAS) is usually asymptomatic, although problems may arise with anesthesia (hypoxia). People who inherit one sickle cell gene and one normal gene have sickle cell trait (SCT).
People with SCT usually do not have any of the symptoms of sickle cell disease (SCD), but they can pass the trait on to their children. People with sickle cell trait are well, and will usually only know about their trait if they are tested for it. Pregnant women and couples planning children may want to know whether they have sickle cell trait, because if both parents have it, their child might inherit SCD. In England, tests for sickle cell trait and SCD are offered to pregnant women and newborn babies.
There is no anemia and in general, people with sickle cell trait enjoy normal life spans with no medical problems related to sickle cell trait. Rarely, extreme conditions such as severe dehydration and high-intensity physical activity can lead to serious health issues, including sudden death, for individuals with sickle cell trait.
Sickle cell disease (SCD – HbSS) usually presents after 6 months of age, as HbF recedes. There are:
- Vaso-occlusive crises with associated infarct pain affecting particularly the bones, joints, and abdominal organs. Aseptic femoral necrosis, dactylitis, renal damage, priapism and retinopathy all may occur. Dactylitis is severe pain that affects the bones of the hands, the feet, or both. It’s often the first symptom of sickle cell disease in babies caused by blocked blood circulation. Symptoms of dactylitis include extreme pain and tenderness, usually with swelling. An episode of dactylitis may last 1 to 4 weeks. Triggers of the vaso-occlusive crisis include Hypoxemia, Dehydration: Acidosis, and Infections.
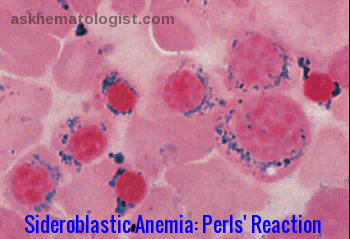
- Anemia may be due to hemolysis, ‘aplastic crises‘ precipitated by parvovirus B19 infection, folate deficiency, and ‘sequestration crises‘ in the liver or spleen.
- Splenomegaly is common in childhood but disappears as the spleen is infarcted. Patients with SCD who have damaged spleens are at risk for serious bacterial infections that can be life-threatening. Some of these bacteria include Pneumococcus, Hemophilus influenza type B, Meningococcus, Salmonella, Staphylococcus, Chlamydia, and Mycoplasma pneumoniae.
- Leg ulceration.
- Acute chest syndrome: Sickled RBCs in the blood vessels of the lungs can cause pulmonary infarcts. This condition is very serious and should be treated immediately at a hospital. Acute chest syndrome often starts a few days after a painful crisis begins. A lung infection may accompany acute chest syndrome. CT pulmonary angiography (CTPA) is indicated in suspected cases of pulmonary embolism (PE).
- Pulmonary hypertension: increasingly recognized as a serious complication of SCD.
- Avascular necrosis of the femoral or humeral head due to vascular occlusion.
- CNS involvement, e.g. stroke.
- Ophthalmologic involvement: ptosis, retinal vascular changes, proliferative retinitis.
- Cardiac involvement: dilation of both ventricles and the left atrium.
- GI involvement: cholelithiasis is common in children; liver may become involved.
- GU involvement: kidneys lose concentrating capacity.
Investigations:
The blood appears normal in sickle cell trait, although the sickle screening test is positive.
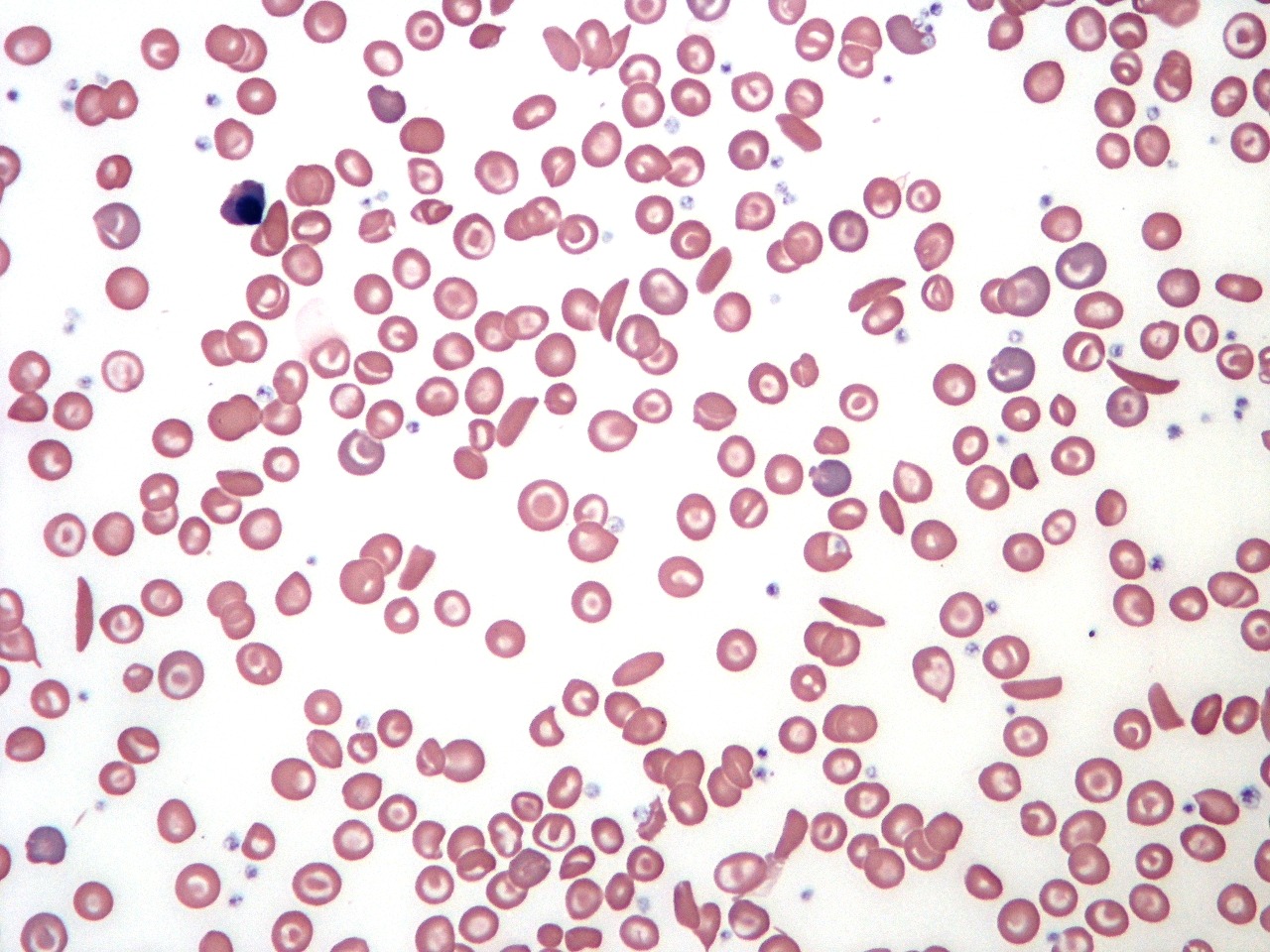
Sickle cell disease is suggested by the typical clinical picture of chronic hemolytic anemia with reticulocytes and sickle cells on the peripheral blood film, and vaso-occlusive crisis. Electrophoresis confirms the diagnosis with the presence of homozygous HbSS (no HbA) and can also document other hemoglobinopathies (eg, HbSC, HbS-beta+ thalassemia).
Laboratory tests used in patients with SCD include the following:
- FBC with differential and reticulocyte count.
- Peripheral blood smear.
- Hb electrophoresis.
- Hemoglobin solubility testing.
- Serum electrolytes.
- Renal function (creatinine, urea, urinalysis).
- LFTs (ALT, indirect and direct bilirubin).
- Pulmonary function tests (transcutaneous O 2 saturation).
- ABGs.
- Blood cultures.
- CSF examination: Consider LP in febrile children who appear toxic and in those with neurologic findings (eg, neck stiffness, + Brudzinski/Kernig signs, focal deficits); consider CT brain scanning before performing LP.
- Secretory phospholipase A2.
N.B. Mandatory screening for HbS at birth in the United States; prenatal testing can be obtained via chorionic villus sampling.
Management:
- Prevention of Crises: patients with SCD should avoid dehydration, hypoxia, acidosis or cold. Infections should be treated promptly.


- Crises are treated by rest, rehydration, management of underlying infection and complications, and administration of analgesics. Oxygen supplementation helps only if the patient has hypoxia. Rapid initiation of opioids for the treatment of severe pain associated with a vaso-occlusive crisis is highly recommended. Patient-controlled analgesia (PCA) is a method of safely administering strong opioids which is controlled by the patient (or a nurse for nurse-controlled analgesia).

- Blood transfusion is indicated in severely affected individuals. Preoperative transfusion therapy should be used to increase hemoglobin levels to 10 g/dL. With continued transfusion, iron overload inevitably develops and can result in heart and liver failure and multiple other complications. Deferasirox (Exjade) has a capacity similar to desferrioxamine (Desferal) in chelating iron, but it is administered orally. Renal toxicity might be a limiting factor in its use, but it is generally safe.
- Folic acid supplements.
- Daily oral prophylactic penicillin (or erythromycin if allergic to penicillin) up to age 5. Many hematologists prefer to continue this antibiotic throughout life in patients with SCD (HbSS).
- There is a strong evidence supporting the efficacy of Hydroxyurea in adults with SCD. It can decrease severe painful episodes, hospitalizations, the frequency of blood transfusions, and the acute chest syndrome. Although the evidence for the efficacy of hydroxyurea treatment for children is not as strong, the emerging data are encouraging. Hydroxyurea increases total and fetal hemoglobin (HbF) in children with SCD. The increase in HbF retards sickling of RBCs. Hydroxyurea also reduces levels of circulating leucocytes, which decreases the adherence of neutrophils to the vascular endothelium. In turn, these effects reduce the incidence of pain episodes and acute chest syndrome episodes.
- Allogeneic Bone Marrow Transplantation (BMT) may be justified in severely affected children, particularly those who have had cerebrovascular incidents.
- Immunization: People with SCD should receive all recommended childhood vaccines. They should also receive additional vaccines to prevent other infections (pneumococcus, meningococcus, influenza).
Other Sickling Disorders
Sickle β thalassemia
Sickling can arise when there is ‘sickle trait’ in association with β thalassemia.
Hemoglobin C
Heterozygotes may have mild sickling episodes and splenomegaly. HbSC is renowned for ocular complications.
Summary:
Sickle cell disease is a genetic blood disorder that affects hemoglobin, the protein in red blood cells that carries oxygen throughout the body. Individuals with sickle cell disease inherit two abnormal hemoglobin genes, one from each parent. This inherited mutation causes the red blood cells to become rigid and sickle-shaped, leading to various complications.
The hallmark of sickle cell disease is the characteristic sickle-shaped red blood cells that can get stuck in small blood vessels, causing blockages that result in pain, organ damage, and a reduced oxygen supply to tissues. This can lead to a range of symptoms, such as severe pain episodes, anaemia, increased risk of infections, and organ damage.
People with sickle cell disease require ongoing medical care to manage symptoms and prevent complications. Treatment may include medications to manage pain, prevent infections, and reduce complications, as well as blood transfusions and stem cell transplants in some cases.
Education, genetic counselling, and early detection through newborn screening are crucial for managing sickle cell disease effectively. Research into new treatments and potential cures continues to advance, offering hope for improved outcomes for individuals living with this challenging condition.
References:
Wang WC (2009). Sickle cell anemia and other sickling syndromes. In JP Greer et al., eds., Wintrobe’s Clinical Hematology, 12th ed., pp. 1038-1082. Philadelphia: Lippincott Williams and Wilkins.
Yawn BP, et al. (2014). Management of sickle cell disease: Summary of the 2014 evidence-based report by expert panel members. JAMA, 312(10): 1033-1048.
Brawley OW, et al. (2008). National Institutes of Health consensus development conference statement: Hydroxyurea treatment for sickle cell disease. Annals of Internal Medicine, 148(12): 932-938.
Serjeant GR. Sickle cell disease. 2nd rev ed. Oxford: Oxford University Press, 1992.
Ohene-Frempong K, Nkrumah FK. Sickle cell disease in Africa. In: Embury SH, Hebbel RP, Mohandas N, et al, eds. Sickle cell disease: basic principles and clinical practice. New York: Raven Press Ltd, 1994.
Olujohungbe A, Howard J. The clinical care of adult patients with sickle cell disease. Br J Hosp Med (Lond). 2008 Nov. 69(11):616-9.
Linguraru MG, Orandi BJ, Van Uitert RL, Mukherjee N, Summers RM, Gladwin MT, et al. CT and image processing non-invasive indicators of sickle cell secondary pulmonary hypertension. Conf Proc IEEE Eng Med Biol Soc. 2008. 2008:859-62.
Keywords:
sickle cell, sickle cell anemia, sickle cell disease symptoms, sickle cell trait, sickle cell crisis, sickle cell symptoms, sickle cell cure, sickle cell anemia treatment, sickle cell trait symptoms, sickle cell anemia cure, sickle cell disease, sickle cell anemia symptoms, sickle cell anemia genetics, sickle cell anemia black people, sickle cell anemia life expectancy, sickle cell anemia and malaria, sickle cell disease symptoms in child, sickle cell disease symptoms pain, sickle cell trait vs disease, sickle cell crisis treatment, sickle cell crisis symptoms, sickle cell crisis triggers, sickle cell crisis labs, sickle cell crisis management, sickle cell crisis causes, sickle cell symptoms in adults.










Thank you for this amazing piece. I learnt a lot from this. Please keep the good work going.
Thank you sir.
Thank you so much sir for detailed information regarding sickle cell disease.