Stomatocytosis
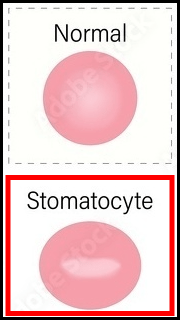
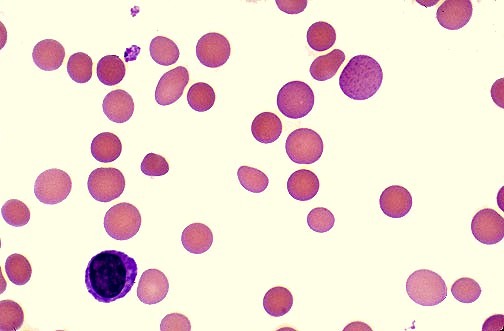
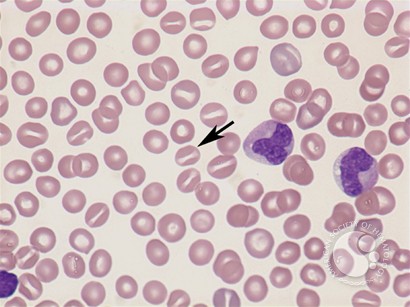
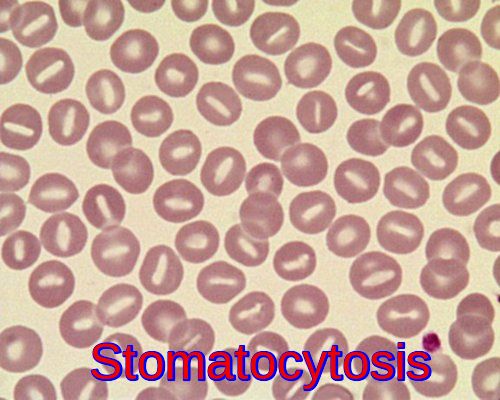 Stomatocytes (RBCs with slit-like central pallor)
Stomatocytes (RBCs with slit-like central pallor)
Stomatocytosis is a rare condition of RBCs in which a mouthlike or slitlike pattern replaces the normal central zone of pallor. These cells are associated with congenital and acquired hemolytic anemia. The symptoms result from anemia and hemolysis.
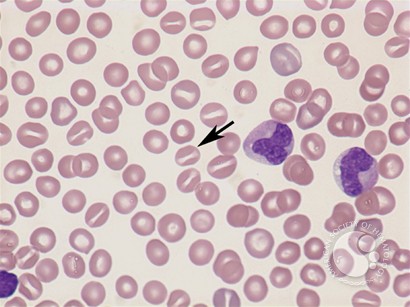
RBCs in which a mouthlike or slitlike pattern replaces the normal central zone of pallor.
The symptoms of stomatocytosis can vary depending on the severity of the disorder. In some cases, people with stomatocytosis may not experience any symptoms at all. However, in more severe cases, the following symptoms may occur:
- Fatigue
- Weakness
- Shortness of breath
- Jaundice
- Enlarged spleen
Stomatocytes are erythrocytes with a central slit or stoma instead of a circular area of pallor when examined on dried smears; they are uniconcave rather than biconcave, giving them a bowl-like appearance. A few stomatocytes may be observed in blood smears prepared from normal individuals, as well as from patients with acute alcoholism and hepatobiliary disease. Large numbers of stomatocytes are associated with very rare hereditary disorders of red cell cation permeability leading to increased or decreased red cell water content.
Hereditary Stomatocytosis comprises two different diseases: the xerocytosis or dehydrated hereditary stomatocytosis and the overhydrated hereditary stomatocytosis. Both are genetic disorders mainly due to an abnormality of red cell membrane permeability to monovalent cations (Na+ and K+) resulting in an alteration in the red blood cell water content. The movement of divalent cations and anions is normal. Typical red blood cells known as stomatocytes (mouth-featured cells) appear in blood smear examination. The clinical manifestation can vary from asymptomatic to severe hemolytic anemia. Hereditary Stomatocytosis shows autosomal dominant inheritance and may cause severe hemolytic anemia presenting very early in life.
Hemolytic anemia with stomatocytosis (up to 40–60%), elevated reticulocyte count, elevated serum bilirubin levels, and reduced serum haptoglobin concentration in children or adolescents are characteristic features of hereditary stomatocytosis.
Stomatocytes have been noted in diverse acquired conditions, including neoplasms, cardiovascular and chronic liver disease, alcoholism, and therapy with drugs, some of which are known to be stomatocytogenic in vitro. In some of these conditions, the percentage of stomatocytes on the peripheral blood smear can approach 100%. However, the clinical significance of this observation is unclear because stomatocytes are absent in most patients with the conditions listed. Furthermore, some stomatocytes can be found in normal individuals (3–5%). The most consistent association is that of stomatocytosis and heavy alcohol consumption.
Splenectomy ameliorates anemia in some cases.
Acquired stomatocytosis with hemolytic anemia occurs primarily with recent excessive alcohol ingestion. Stomatocytes in the peripheral blood and hemolysis disappear within 2 weeks of alcohol withdrawal. Stomatocytosis could also be seen in thalassemia, neoplastic, cardiovascular or hepatobiliary disease including acute alcoholism and during therapy with certain drugs some of which are known to be stomatocytogenic in vitro.
Among the common drugs associated with stomatocytogenic effects:
- Hydroxyurea
- Propranolol
- Quinine
- Valproic Acid
- Phenothiazines e.g. chlorpromazine
- Cytosine arabinoside (Ara-C)
- 6-thioguanine
There is no cure for hereditary stomatocytosis, but treatment may be recommended to manage symptoms. This may include blood transfusions, medications to control symptoms, and in severe cases, splenectomy.
References:
Patrick G. Gallagher; Faramarz Naeim; and Bertil Glader. Red Blood Cell Membrane Disorders. https://www.sciencedirect.com/science/article/pii/B9780123838346000768
Red blood cell morphology. Shape of red blood cell. https://stock.adobe.com/ie/images/red-blood-cell-morphology-shape-of-red-blood-cell-spherocyte-ovalocyte-sickle-cell-target-cell-stomatocyte-echinocyte-acanthocyte-schistocyte-and-tear-drop/500976159
Neville AJ, Rand CA, Barr RD, Mohan Pai KR. Drug-induced stomatocytosis and anemia during consolidation chemotherapy of childhood acute leukemia. Am J Med Sci. 1984 Jan-Feb;287(1):3-7. doi: 10.1097/00000441-198401000-00001. PMID: 6608270.
Gallagher, P. G. (2013). Red cell membrane disorders. Hematology Am Soc Hematol Educ Program, 2013(1), 16-21.
Bruce, L. J., & Cope, D. L. (2012). Inherited erythrocyte membrane disorders–often overlooked diagnoses. Hematology Am Soc Hematol Educ Program, 2012, 461-466.
Andolfo, I., Russo, R., & Iolascon, A. (2015). Hereditary stomatocytosis: an underdiagnosed condition. American journal of hematology, 90(1), 82-86.
Keywords:
what is stomatocytosis, stomatocytosis causes and symptoms, stomatocytosis treatment.





How do they test for for Stomatocytosis? My 25 year old daughter has a chronic illness Endometriosis stage 4( which has not got the amount of research it should) and she has symptoms of Anemia.. Her hematocrit is 32.5 and hemoglobin is 10.5 and her latest blood test says Stomatocytes are present but no percentage. Most doctors want to blame everything on her Endometriosis but anemia is not a symptom. So we just want to make sure we arent missing anything. Thank you for any information or advice.
Hi Patricia,
Stomatocytes are identified on the blood smear and can be seen in a variety of medical conditions especially liver disease and excess alcohol consumption. I don’t think there is a direct link between endometriosis and stomatocytosis. Anemia associated with endometriosis could be secondary to iron deficiency caused by heavy periods.
BW,
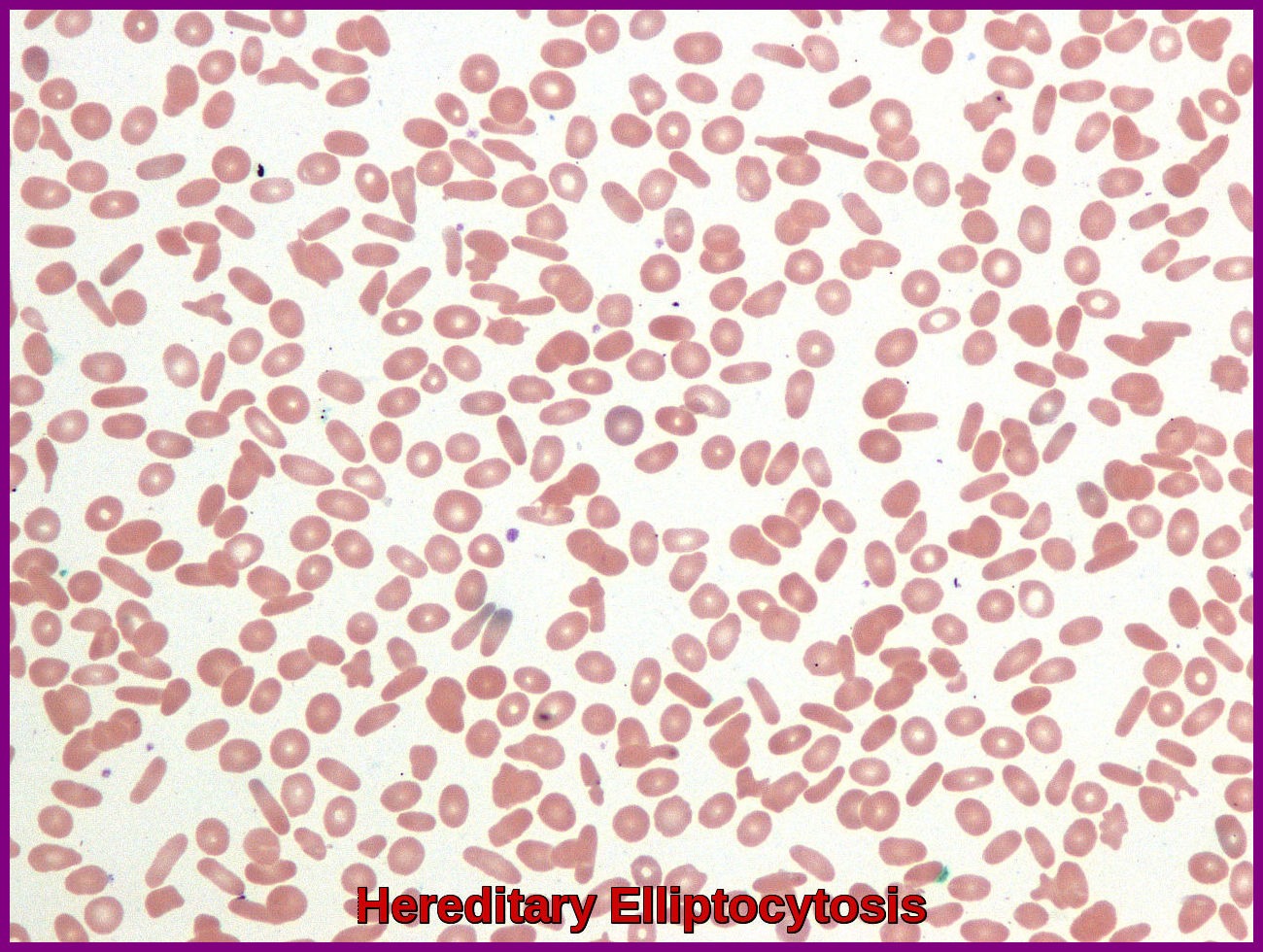
I have had various blood tests and a blood smear test said occasional target cells. Image result for Stomatocytes
Stomatocytes and elliptocytes present. Can you cause this to happen if you work too much, dont sleep enough, or are stressed or dont eat properly, why is my blood test showing this please and what does it mean for me? can it go and turn to a normal blood test again. I dont drink or smoke. Thank you. Michele
Hi Michele,
Thank you for your comment.
Some stomatocytes and elliptocytes can be seen in normal individuals and they don’t have any clinical significance as long as you are not anemic or having chronic liver disease. You can simply ignore them.
BW,
Can i ask what is the possible treatment for the acquired stomatocytes.
Hi,
Thanks for your comment.
The treatment of the acquired stomatocytosis is the treatment of the underlying cause, e.g. liver disease, excessive alcohol ingestion, etc.
BW,
I have had various blood test, and it said i have Silent congenital ovalocytosis and stomatocytosis and reactive leucocytosis.
What is the possible treatment and can it go and turn to a normal blood test again.
Hi Louie,
Thanks for your comment.
At present, there is no specific treatment for Hereditary Stomatocytosis. Many patients with hemolytic anemia take folic acid (vitamin B9) since the greater turnover of cells consumes this vitamin. During crises, transfusion may be required. Unlike hereditary spherocytosis, splenectomy is not indicated.
BW,
I know very little about a childhood blood disorder that may be hereditary stomatocytosis. I recall being told that I could be found eating dirt as a toddler and that I was transfused in the early 1970s. Throughout life (now 53, male), I have either been anemic or on the low end of the normal range and had low iron level readings in blood tests. A year ago, I had iron infusions and took an iron supplement. Energy level and blood test greatly improved. I discontinued the supplement when my iron level was in the upper end of the range (about 9 months ago). Endoscopy was unremarkable. One benign polyp on colonoscopy. No alcohol for three years. Had been a drinker (at times heavy) for 30 years. Stomatocytosis observed by hematologist over last several years. Iron levels falling since discontinuation of supplements. Feeling fatigue and chest tightness that improves with exercise. I have asthma, but I actually breath better the more I exercise. Sleep apnea well controlled with biPAP. I walk 20+ miles a week. Also have Selective IgM deficiency, which makes me very prone to respiratory infections. I live in a humid environment, and lately feel like I just can’t breath. Makes me anxious. Seeing the hematologist for tests again soon. Suspect I have anemia and low iron. No obvious bleeding. Slightly fatty liver, but not awful. Enzymes in normal range. A1C slightly elevated but not diabetic. I do take omeprazole and atorvastatin. Also Symbicort and albuterol. What else should I be asking my doctors? My blood pressure is slightly high, GP wants me to consider medication for that. I want to stay active. Doctors seem puzzled when I say the chest tightness goes away when I’m walking hard. I don’t think it’s asthma, and I did feel really good when I know my iron and hemoglobin were higher.
Hi MW,
Thanks for your comment.
If you have excluded blood loss as a possible cause of your iron deficiency anaemia, I would suggest to also exclude malabsorption of iron from the bowel by checking Anti-endomysial antibody (EMA) and tissue transglutaminase antibody (tTG) levels.
BW,
Hello,
I had a CBC and it showed slight stomatocytes, however, I had a repeat test done three weeks later, but I do not see anything that suggests stomatocytes are still present. What could that mean?
Thank you!
Hi Rose,
Thanks for your comment.
Acquired Stomatocytosis can be found in normal individuals (3–5%).
The most consistent association is between stomatocytosis and chronic liver disease and/or heavy alcohol consumption.
They shouldn’t cause concern if the blood indices are normal and you are not anemic.
BW,
Thank you very much for your response.
You’re welcome!
Hello.
I have been told that I have MDS following blood tests done after a GI bleed. The blood test results showed: RBC 3.81 – MCV 103.6 – MCH 35.2 – PLATELETS 91.
Blood tests showed macrocytosis with stomatocytes present.
Doctor says that I have MDS.
Bone marrow biopsy results showed ? fingerprinting film in both liquid and ‘hard’ marrow test of lymphocytes being present?
Alcohol intake really quite low.
Non smoker for 25 years.
Low platelet count has been present for 30 years following a massive viral infection acquired whilst on holiday in the Gambia resulting in 6 months of work. (unheard of to take time off work for me)
Was contacted by the NHS following a visit to the hotel in London at the same time that the Russian ‘spy’ was in contact with polonium poisoning????
Any comments would be gratefully accepted please.
Hi Lesley,
Thank you for reaching out. I understand your concern about the MDS diagnosis.
To provide a more accurate assessment, I would need to review the complete bone marrow biopsy report.
Additionally, it’s important to rule out other potential causes of macrocytosis such as B12/Folate deficiency, liver disease, and underactive thyroid.
Please send me the complete report so that I can assist you further.
Your long-standing low platelets could be immune-mediated or drug-related.
BW,
I have had stomacytosis for over a year, but recently discovered my phosphorous has been around 2 or less as well. Extreme fatigue, bone weakness, kidney stones, confusion, brain fog, spleen calcifications, tinnitus and straightening of the cervicel lordosis
My coworker who’s a doctor sees I bring Diet Coke everyday to work and prescribed me phosphate 250 drug. I am confused how a drink that has phosphoric acid can deplete my phosphorus and also cause stomacytosis. I just started it today and I am hoping this will fix my chronic fatigue and brain fog. I switched to light colored diet sodas instead.
Just haven’t seen much online about this Diet Coke and low phos and stomacytosis problem. And been hunting a year for this problem with no answers till recently.
I feel alone in this problem as I haven’t seen others talk about this, was wondering if you have seen anything similar?
Hi Tora,
I’m sorry to hear about your health challenges. It’s understandable that you’re feeling confused and frustrated.
As is well known, cola represents a strong exogenous source of phosphate, due to its high phosphorus content (about 15–20 mg/dL), more than other carbonated soft drinks. High consumption of cola can cause a sudden change in the pH gastric values as a consequence of the strong cola acidity (pH 1.8). The effect of cola on calcium concentration seems to be connected to its high phosphate concentration. Indeed, when the cola drink is ingested, a considerable decrease in calcium concentration and, of course, an increase in phosphorus concentration is observed.
However, I don’t think there is a direct link between cola consumption and stomatocytosis. If you don’t drink alcohol in excess, I would suggest checking your liver function tests, including gamma GT, and having an ultrasound scan on your liver.
BW
Dr. M Abdou
Hello; My wife passed away. But, at first, doctors thought she had cirrhosis. Although her LFTs were normal, she had a high Total Bilirubin, and Normal direct billi, with slightly low albumin. A liver biopsy showed Fatty liver, 1 of 3 ballooning, and grade 1 fibrosis.
She had gone into the hospital with a bleed from Eshphugeal erosion caused by bile reflux. For one reason or another, they treated her with 2g of Cefraxone and 1g of Vancomycin. She developed a severe AKI and had to be admitted.
They then ran into issues, that she needed a blood transfusion every 4-5 days. A GI scope found no bleeds, a colonoscopy found no bleeds, and stool testing showed no blood present.
Her Albumin levels were bouncing all over the planet from normal to low back to normal to low. One day it would be normal the next below normal, a few days later. Back up again.
Blood Smears showed a high level of Stomatocytes and Polychromasia. Her liver was slightly enlarged at 15.6 cm. Spleen Normal, Dopler showed normal portal flow.
Her ammonia levels were normal.
Could the Hemolysis going on be a reaction to the Cefraxone?
She died due to Renal failure from a toxic vancomycin trough level of 86.8.
Hi Charles,
I extend my deepest condolences for the loss of your wife.
I appreciate you reaching out, and I understand the importance of clarifying the circumstances surrounding her passing.
It’s crucial to consider the complexities involved in such cases.
Immune hemolytic anemia can indeed be a rare adverse effect of medications like ceftriaxone and vancomycin.
However, implicating them directly requires a thorough assessment of the clinical context.
Regarding vancomycin-induced acute kidney injury (AKI), although many cases are reversible, the association with a higher incidence of end-stage kidney disease and increased mortality rates underscores the need for a careful evaluation of the overall clinical picture.
The presence of stomatocytes and polychromasia in the blood raises concerns about potential liver disease and the release of immature red blood cells from the bone marrow (reticulocytes) due to hemolysis or blood loss. Performing a direct Coombs test as part of routine investigations is a prudent step to differentiate between immune and non-immune hemolysis, which might be contributory to the elevated indirect bilirubin in your wife’s case.
Given the complexity of the situation, it is challenging to draw definitive conclusions based solely on the information provided. The differential diagnosis should include considerations of microangiopathic hemolytic anemia (MAHA) which carries a poor prognosis.
Best regards,
Dr. M Abdou