Spherocytosis
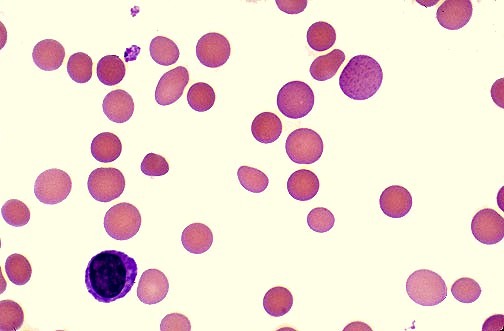
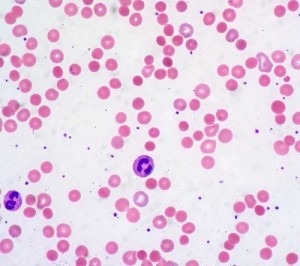
Hereditary Spherocytosis (HS) is a disorder of the red cell membrane inherited usually in an autosomal dominant pattern. In this condition, the red cells are more rigid and fragile than normal. They are spherocytic, appearing small, deeply stained on blood smears, and have osmotic fragility. Spherocytes are found in all hemolytic anemias to some degree. Hereditary spherocytosis and autoimmune hemolytic anemia are characterized by having only spherocytes. Spherocytosis most often refers to hereditary spherocytosis.
Hereditary Spherocytosis results from defects in the structural proteins of the red blood cell (RBC) membrane, particularly spectrin, ankyrin, and band 3 protein. This leads to the formation of spherical RBCs, reducing their flexibility and increasing vulnerability to splenic sequestration and destruction. Spherocytosis can manifest with varying degrees of severity, from asymptomatic cases to severe hemolytic anemia.
A normal red blood cell can live for up to 120 days. A red blood cell with hereditary spherocytosis might live for as few as 10 to 30 days.
Diagnosis:
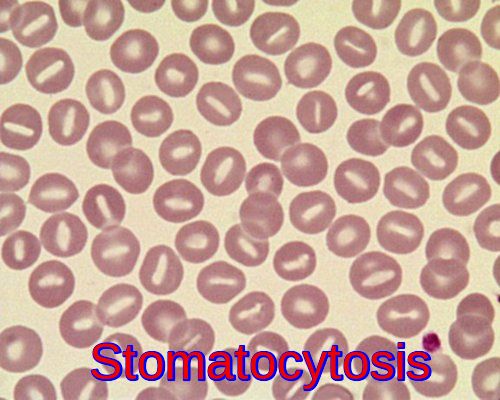
Diagnosis of hereditary spherocytosis involves a combination of clinical, laboratory, and imaging studies. Blood smear analysis typically reveals characteristic spherocytes and osmotic fragility testing can confirm increased RBC fragility. Molecular genetic testing is crucial for identifying specific mutations associated with spherocytosis.
The spleen is usually enlarged and palpable.
Anemia is usually mild, but the Hb may fall considerably with intercurrent infections (aplastic crises) or during periods of increased splenic sequestration (hemolytic crises).
Folate deficiency is caused by increased bone marrow requirement.
Jaundice is usually mild, if detectable, but may rarely cause kernicterus.
Pigmented gallstones occur in approximately half of untreated patients.
Abnormally low hemoglobin A1C (Hb A1C) levels because the life span of the red blood cells is decreased, providing less time for the non-enzymatic glycosylation of hemoglobin. Thus, the Hb A1C will be lower than expected even with high overall blood sugar.
Management:
Management of hereditary spherocytosis aims to alleviate symptoms, prevent complications, and improve overall quality of life.
Folate supplementation is often recommended to support increased erythropoiesis.
Splenectomy may be considered in severe cases but the decision requires careful consideration of risks and benefits. Splenectomy improves the hemolysis and is performed if indicated, preferably after childhood.
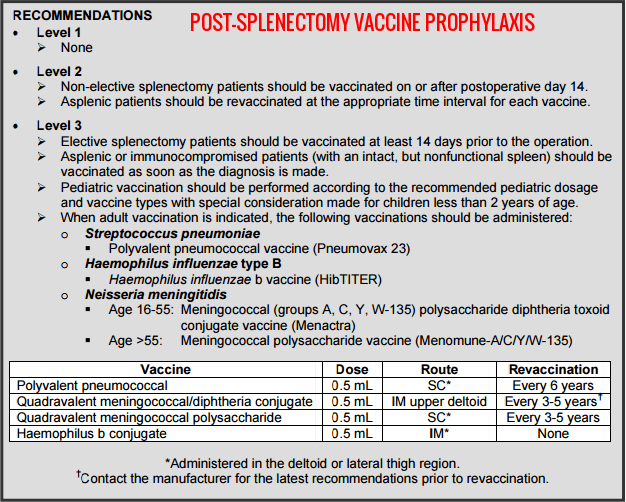
Penicillin should be given to splenectomized patients and they should be vaccinated to decrease the risk of overwhelming post-splenectomy sepsis due to organisms such as Streptococcus pneumoniae, Haemophilus influenzae type B, and Neisseria meningitidis.
Red blood cell transfusions may be required in severe cases of anemia, particularly in the first years of life or during infections and pregnancy. If red blood cell transfusions are needed repeatedly, iron chelating therapy may be required to reduce iron overload.
Spherocytes are also seen in some immune-mediated hemolytic anemias.
Overall, the long-term outlook (prognosis) for people with hereditary spherocytosis (HS) is usually good with treatment.
Conclusion:
Spherocytosis is a complex disorder with diverse clinical manifestations. Early diagnosis and appropriate management are crucial for improving outcomes and preventing complications. Continued research into the genetic basis of spherocytosis may pave the way for targeted therapies in the future.
References:
Bolton-Maggs PH, Langer JC, Iolascon A, et al; General Haematology Task Force of the British Committee for Standards in Haematology. Guidelines for the diagnosis and management of hereditary spherocytosis – 2011 update. Br J Haematol. 2012;156:37-49.
Perrotta S, Gallagher PG, Mohandas N. Hereditary spherocytosis. Lancet. 2008;372:1411-1426.
Post-splenectomy vaccine prophylaxis Department of Surgical Education, Orlando Regional Medical Center
Kutter, D; Thoma, J (2006). “Hereditary spherocytosis and other hemolytic anomalies distort diabetic control by glycated hemoglobin.”. Clinical laboratory. 52 (9-10): 477–81.
British Committee for Standards in Haematology. Guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen. BMJ. 1996;312:430-434.
Spherocytosis. https://healthjade.com/spherocytosis/ via @Health Jade
Robert S. Hillman; Kenneth A. Ault; Henry M. Rinder (2005). Hematology in clinical practice: a guide to diagnosis and management. McGraw-Hill Professional. pp. 146–. ISBN 978-0-07-144035-6
Hereditary Spherocytosis. Shafqat Shah, Roger Vega. Pediatrics in Review May 2004, 25 (5) 168-172; DOI: 10.1542/pir.25-5-168








Hi, please could you assist me with info, my son hase spherocytosis and my consern is nou that the schools are opening, can i take the chance to send him in this covid 19 epidemic. Please help me with advice…
Hi Danielle,
Thank you for your comment.
If he is not splenectomised, he doesn’t meet the high risk criteria for contracting coronavirus (COVID-19) and he doesn’t need shielding unless he has another medical condition or on medications which could compromise his immune system.
BW,