Checkpoint Inhibitors
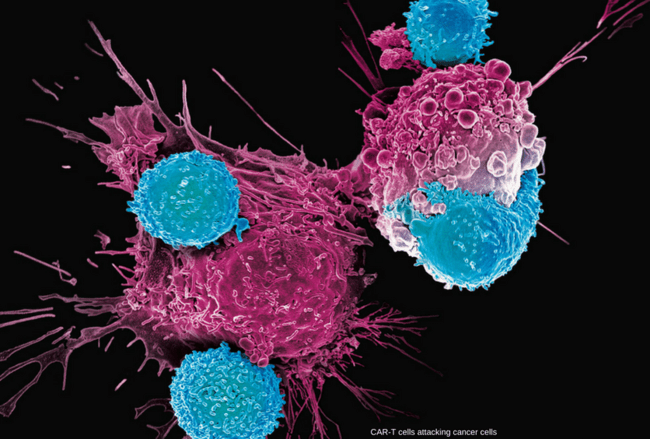
An important part of the immune system is its ability to tell between normal cells in the body and those it sees as “foreign”. This lets the immune system attack the foreign cells while leaving the normal cells alone. Unfortunately, immune system doesn’t always recognize cancer as a threat.
Immune system uses “checkpoints” – molecules on certain immune cells that need to be activated (or inactivated) to start an immune response.
Cancer cells sometimes find ways to use these checkpoints to avoid being attacked by the immune system. They can hide by fooling immune cells into thinking they are not foreign at all. To determine friend or foe, immune cells check for a protein. If they find it on cancer cells, they appear as friends.
Drugs that target these checkpoints “checkpoints inhibitors” hold a lot of promise as cancer treatments. They do just what the name suggests –they block the checkpoint that looks for friend or foe. Seeing no friend because they are blocked, immune cells mount a defense.
Immune checkpoint inhibitors are monoclonal antibodies that block proteins, called “checkpoints,” expressed by tumor cells to inhibit the immune response. The development of this therapy for hematologic cancers has lagged behind that of solid tumors, but new data at the 2015 ASH annual meeting suggest the promise may be similar.
In solid tumors, several checkpoint inhibitors have now been granted regulatory approval for single-agent use in advanced disease. The most recent approvals, granted to both nivolumab and pembrolizumab, were for single-agent use in advanced non-small cell lung cancer. As yet, no checkpoint inhibitor has been granted an indication for a hematologic cancer or lymphoproliferative disorder, but it appears that at least some of the approvals, when they are granted, will be for a checkpoint inhibitor in combination with a second agent.
Checkpoint inhibitors scored some impressive successes in recent years, particularly in some patients with metastatic melanoma, metastatic non-small cell lung cancer (NSCLC), advanced renal cell carcinoma or classical Hodgkin lymphoma, and are showing promise in clinical trials involving patients with other types of cancer.

Checkpoint inhibitors block normal proteins on cancer cells, or the proteins on the T cells that respond to them
Drugs that target The programmed cell death-1 (PD-1) receptor or one of its ligands, (PD-L1):
PD-1 is a checkpoint protein on immune T cells. It normally acts as a type of “off switch” that helps keep the T cells from attacking other cells in the body. It does this when it attaches to PD-L1, a protein on some normal (and cancer) cells. When PD-1 binds to PD-L1, it basically tells the T cell to leave the other cell alone. Some cancer cells have large amounts of PD-L1, which helps them evade immune attack.
Monoclonal antibodies that target either PD-1 or PD-L1 can boost the immune response against cancer cells and have shown a great deal of promise in treating certain cancers.
PD-1 inhibitors: Examples of drugs that target PD-1 include:
Pembrolizumab (Keytruda)
Nivolumab (Opdivo)
These drugs have been shown to be helpful in treating several types of cancer, including metastatic melanoma, non-small cell lung cancer, advanced renal cell carcinoma, head and neck cancers, and Hodgkin lymphoma. They are also being studied for use against many other types of cancer.
PD-L1 inhibitors: An example of a drug that targets PD-L1 is:
Atezolizumab (Tecentriq)
This drug can be used to treat bladder cancer, and is also being studied for use against other types of cancer.
One concern with all of these drugs is that they can allow the immune system to attack some normal organs in the body, which can lead to serious side effects in some people.
Common immune-related adverse events of these drugs can include fatigue, cough, nausea, loss of appetite, skin rash, and itching. Less often they can cause more serious problems in the lungs, intestines, liver, kidneys, endocrine glands, or other organs.
Many other drugs that target either PD-1 or PD-L1 are now being tested in clinical trials as well, both alone and combined with other drugs.
Drugs that target Cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4):
CTLA-4 is another protein on some T cells that acts as a type of “off switch” to keep the immune system in check.
CTLA-4 inhibitors:
Ipilimumab (Yervoy) is a monoclonal antibody that attaches to CTLA-4 and stops it from working. This can boost the body’s immune response against cancer cells.
This drug is used to treat metastatic melanoma. It is also being studied for use against other cancers.
Because ipilimumab affects the immune system, it can sometimes cause serious or even life-threatening side effects. In fact, compared to drugs that target PD-1 or PD-L1, serious side effects seem to be more likely with ipilimumab.
Conclusion:
Immune checkpoint blockade using inhibitors of cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and programmed cell death-1 (PD-1) has shown clinically significant antitumor response and has been approved for the treatment of malignant melanoma and squamous non-small cell lung cancer (NSCLC). These immunotherapies are associated with unique set of toxicities termed immune-related adverse events (irAEs) that are very different from toxicities observed with conventional cytotoxic chemotherapy. Prompt recognition and initiation of appropriate management, usually in the form of immunosuppression, usually results in complete reversibility, but failing to do so can lead to severe toxicity or even death. Clinical algorithms describing the management of common irAEs have been published based on clinical trial information and experience in metastatic melanoma with ipilimumab, a human IgG1 monoclonal antibody that binds to CTLA-4 and blocks T cell inhibition. The most common irAEs reported with ipilimumab are dermatologic toxicity, diarrhea/colitis, hepatotoxicity, and endocrinopathies, although other sites can also be affected. Similar irAEs have been observed with agents targeting PD-1. Nivolumab and pembrolizumab are humanized monoclonal antibodies that bind to PD-1 and prevent T cell inactivation. Ipilimumab, pembrolizumab, and nivolumab are approved by the Food and Drug Administration (FDA) for the treatment of advanced melanoma; nivolumab was also recently approved for metastatic squamous NSCLC.
Temporary immunosuppression with corticosteroids, tumor necrosis factor-alpha antagonists, mycophenolate mofetil, or other agents can be an effective treatment for anti-CTLA-4 and anti-PD-1/PD-L1 immune-related adverse events.
References:
Immune checkpoint inhibitors to treat cancer http://www.cancer.org/treatment/treatmentsandsideeffects/treatmenttypes/immunotherapy/cancer-immunotherapy-immune-checkpoint-inhibitors Accessed: August 2016.
Theodore Bosworth Checkpoint Inhibitors in Hematologic Cancers: Overview http://www.medscape.com/viewarticle/857469 Accessed: January 2016.
Postow MA. From the Memorial Sloan Kettering Cancer Center, New York, NY; Weill Cornell Medical College, New York, NY. Managing immune checkpoint-blocking antibody side effects: Am Soc Clin Oncol Educ Book. 2015:76-83. doi: 10.14694/EdBook_AM.2015.35.76. review. PMID: 25993145.
Villadolid J, Amin A. Immune checkpoint inhibitors in clinical practice: update on management of immune-related toxicities. – PubMed – NCBI https://www.ncbi.nlm.nih.gov/pubmed/26629425 Accessed: October 2015.
Dana-Farber Cancer Institute What Is a Checkpoint Inhibitor? Immune Checkpoint Inhibitor Definition http://blog.dana-farber.org/insight/2015/09/what-is-a-checkpoint-inhibitor/ Accessed: July 2016.
David Charbonneau Your microbiome and cancer https://eyeviewkamloops.wordpress.com/tag/checkpoint-inhibitors/ Accessed: June 2016.










After I read the article, especially when I am interested in the field of immunity and how to strengthen immunity in the body, what are the latest statistics for this treatment? And what are the countries that have used such drugs
Hi Mohamed,
Thank you for your comment.
Checkpoint inhibitors are in use in the UK for several years now. In Hematology we use them in relapsed or refractory classical Hodgkin lymphoma e.g. nivolumab or pembrolizumab.
BW,