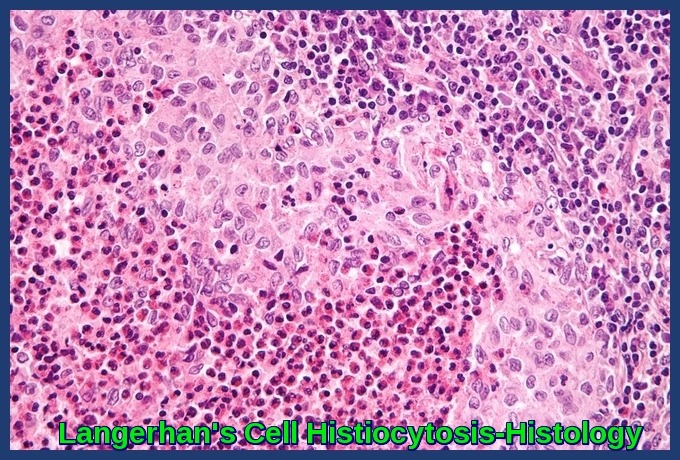
Langerhan’s Cell Histiocytosis
Langerhan’s Cell Histiocytosis (LCH), also called Histiocytosis X, is a group of diseases ranging from the relatively benign unifocal eosinophilic granuloma, to the multifocal variant, to the very malignant diffuse histiocytic infiltration previously known as the Letterer-Siwe syndrome which is frequently fatal.
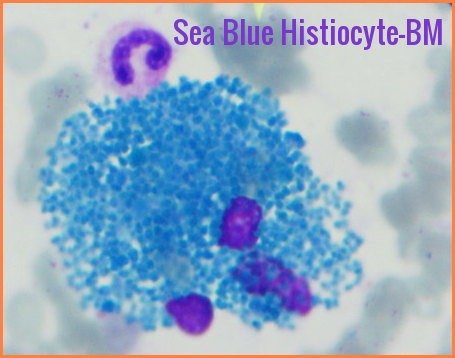
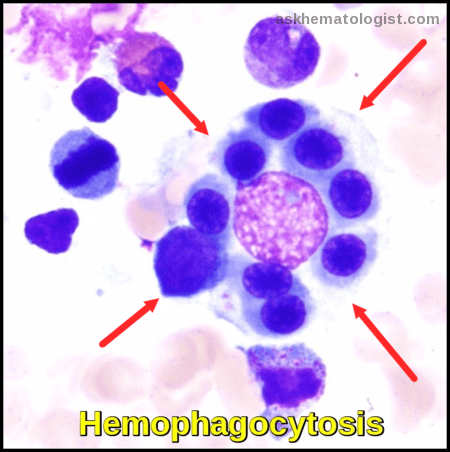
This disorder is characterized by an abnormal increase in certain immune cells called histiocyte cells. Histiocyte cells are a form of white blood cells that help the immune system destroy foreign materials and fight infection. The extra immune cells produced by this condition may form tumors with infiltration into organs locally or diffusely.
Langerhans cell histiocytosis historically was thought of as a cancer-like condition, but more recently researchers have begun to consider it an autoimmune phenomenon in which immune cells begin to overproduce and attack the body instead of fighting infection.
Most cases affect children between 1 and 15 years old, with the majority of new cases in children between 5 and 10.
Langerhan’s Cell Histiocytosis provokes a non-specific inflammatory response, which includes fever, lethargy, and weight loss. Organ involvement can also cause more specific symptoms.
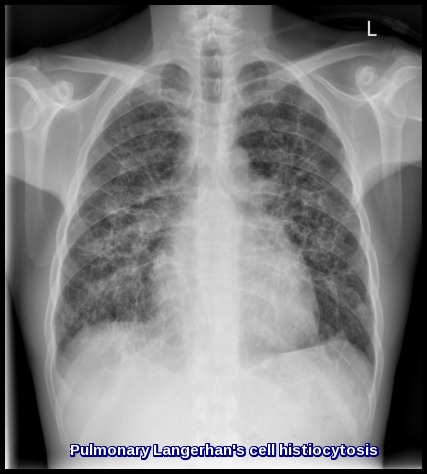
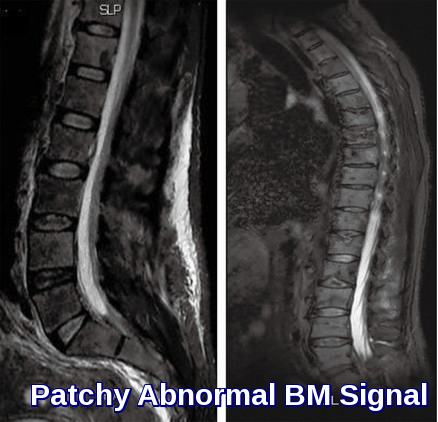
Manifestations may include lung infiltrates; bone lesions; skin rashes; and hepatic, hematopoietic, and endocrine dysfunction.
Diagnosis is based on biopsy.
Factors predicting a poor prognosis include age < 2 yr and dissemination, particularly involving the hematopoietic system, liver, lungs, or a combination.
Treatment includes supportive measures, chemotherapy, local treatment with surgery or radiation therapy as indicated by the extent of disease.
Systemic chemotherapy is indicated for multisystem disease and cases of single-system disease not responsive to other treatment. The combination of cytotoxic drugs and systemic steroids is generally effective. Low-to-moderate doses of methotrexate, prednisone, and vinblastine are used.
Some patients require hormone replacement for diabetes insipidus (DDAVP) or other manifestations of hypopituitarism.
References:
Komp DM. Historical perspectives of Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1987 Mar. 1(1):9-21.
Merad M, Ginhoux F, Collin M. Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nat Rev Immunol. 2008 Dec. 8(12):935-47.
Egeler RM, van Halteren AG, Hogendoorn PC, Laman JD, Leenen PJ. Langerhans cell histiocytosis: fascinating dynamics of the dendritic cell-macrophage lineage. Immunol Rev. 2010 Mar. 234(1):213-32.




Hey, It really is an incredibly fantastic and informative website. Good to discover your site Very well article! I’m simply in love with it.