Polycythemia Rubra Vera
Polycythemia Rubra Vera (PRV) is a chronic myeloproliferative neoplasm characterized by an increased red blood cell (RBC) production and RBC mass often manifested as an increased hematocrit (Hct). There is a malignant transformation of the multipotential stem cell with excess production of red blood cells in the bone marrow and blood, causing the blood to thicken. The number of white blood cells and platelets may also increase. The extra blood cells may collect in the spleen and cause it to become enlarged. They may also cause bleeding problems and make clots form in blood vessels.
Extramedullary hematopoiesis may occur in the spleen, liver, and other sites with the potential for blood cell formation. There is no Philadelphia chromosome.
The major symptoms are related to hypertension or vascular abnormalities caused by the increased red cell mass. The cause is unknown. The ICD-10-CM Diagnosis Code for Polycythemia Rubra Vera (PRV) or Primary Polycythemia Vera is D45. With currently available treatment, the median survival exceeds 10 years (WHO 2001).
PRV is the most common of the myeloproliferative neoplasms, with incidence increasing with age. PRV may be slightly more common in men. The mean age at diagnosis is around 60 years. The disease is very rare in children.
Clinical Features:
Develop gradually and include:
- Headaches, dizziness, tinnitus and visual problems.
- The face may be red (plethoric), and the retinal veins engorged. The palms and feet may be red, warm, and painful.
- Thrombotic episodes e.g. (neurologic deficits with stroke or transient ischemic attack, DVTs, unilateral vision loss with retinal vascular occlusion).
- Bleeding episodes, especially peptic ulcers.
- Generalized pruritus, particularly after a hot bath.
- Gout.
- Hepatomegaly is common, and splenomegaly is present in 75% of cases.
- One-third of patients are hypertensive.
- Hypermetabolism can cause low-grade fevers and weight loss and suggests disease progression.
Investigations:
- Raised Hb.
- Raised red cell mass. This is essential for the diagnosis to differentiate it from pseudo-polycythemia (relative polycythemia) due to a low plasma volume.
- White cell count is usually raised.
- Platelet count is often raised.
- NAP score is raised.
- JAK2 V617F mutation.
- JAK2 exon 12 mutation.
- CXR.
- Abdominal USS.
- In some cases, the diagnosis of PRV must be made by carefully excluding Secondary Polycythemia. This includes a CXR, IV urogram, blood gases, Hb electrophoresis and O2 dissociation curve.
Diagnostic criteria for PRV as per the 2008 revised World Health Organization (WHO) guidelines include both major and minor criteria. Diagnosis requires the presence of both major criteria and one minor criterion or the presence of the first major criterion together with two minor criteria.
Major WHO criteria are as follows:
- Hemoglobin >18.5 g/dL in men and >16.5 g/dL in women, or other evidence of increased red blood cell volume.
- Presence of JAK2 V617F or other functionally similar mutation, such as JAK2 exon 12 mutation.
Minor WHO criteria are as follows:
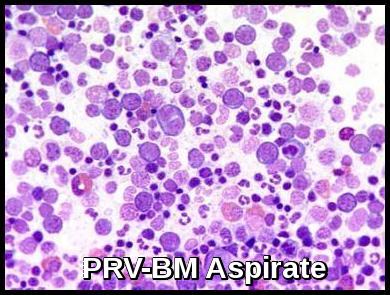
- Bone marrow biopsy showing hypercellularity for age with trilineage growth (panmyelosis) with prominent erythroid, granulocytic, and megakaryocytic proliferation.
- The serum erythropoietin level is below the reference range for normal.
- Endogenous erythroid colony formation in vitro.
JAK2 V617F mutation and erythropoietin (EPO) level are key in diagnosing erythrocytosis. If the JAK2 V617F mutation is positive and the EPO level is low, then it confirms the diagnosis of PRV (JAK2 V617F mutation is positive in 97% of PRV patients).
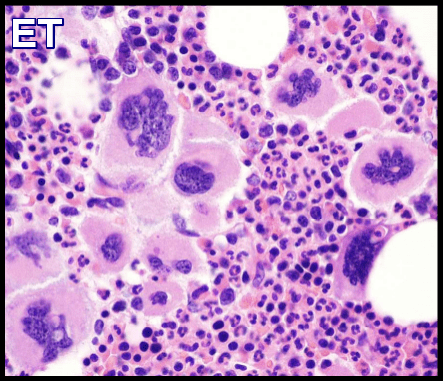
JAK2 mutations also occur in about 60% of patients with essential thrombocythemia. In patients who are positive for JAK2 and whose hemoglobin/hematocrit level is diagnostically equivocal, bone marrow examination is necessary to distinguish the two conditions.
If the JAK2 V617F mutation is absent but the EPO level is low, then testing for JAK2 exon 12 and 13 mutations would be helpful for making a diagnosis of PRV in the 2-3% of PRV patients who are negative for JAK2 V617F mutation.
Patients who are negative for JAK2 mutations and have a normal or high EPO level have secondary polycythemia.
Treatment:
Repeated phlebotomies (venesections) aiming to keep Hct < 0.45
Cytoreductive therapy e.g. Hydroxyurea (Hydroxycarbamide). In patients who are refractory to or intolerant of hydroxyurea, interferon-alpha can be used as an alternative. Busulfan is also an option for patients older than 65 years.
Aspirin, 75 mg daily, unless contraindicated by major bleeding or gastric intolerance.
Allopurinol to prevent gout.
JAK inhibitors: the JAK1/2 inhibitor Ruxolitinib (Jakavi) is approved for treating PRV in patients who have had an inadequate response to or are intolerant of hydroxyurea.
Radioactive phosphorus (rarely used).
Control of blood pressure if raised.
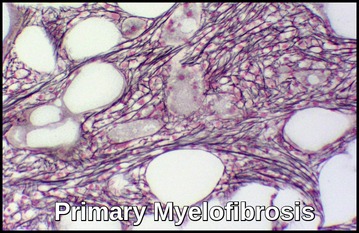
Untreated PRV is fatal within several years. The long-term risks of PRV include acute leukemia and myelofibrosis transformation, which occurs in fewer than 5% and 10% of patients, respectively, at 10 years. Current treatment modalities do not change these outcomes. Instead, treatment for PRV is intended to decrease the risk of arterial and venous thrombotic events, which could be approximately 20%.
Summary:
Polycythaemia Rubra Vera (PRV) is characterized by the overproduction of red blood cells in the bone marrow without any identifiable cause. These cells accumulate in the bone marrow and in the bloodstream, where they increase the blood volume and cause the blood to become thicker or more ‘viscous’ than normal. In many people with polycythemia rubra vera, too many platelets and white cells are also produced. JAK2 V617F mutation and erythropoietin (EPO) level are key in diagnosing the disease. The JAK2 V617F mutation is positive in 97% of PRV patients, and the EPO level is low. Management aims to control hematocrit levels and reduce the risk of thrombotic events. Therapeutic phlebotomy is a standard approach to lower blood cell counts. Additionally, medications like hydroxyurea or ruxolitinib may be prescribed. PRV patients are at an increased risk of thrombosis, bleeding, and transformation to myelofibrosis or acute leukemia.
References:
Adamson JW, Fialkow PJ, Murphy S, et al. Polycythemia vera: stem-cell and probable clonal origin of the disease. N Engl J Med. 1976;295:913-916.
James C, Ugo V, Le Couedic JP, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434:1144-1148.
NewLandolfi R, Marchioli R, Kutti J, et al. Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med. 2004;350:114-124.
NewVannucchi AM, Kiladjian JJ, Griesshammer M, et al. Ruxolitinib versus standard therapy for the treatment of polycythemia vera. N Engl J Med. 2015;372:426-435.
NewMarchioli R, Finazzi G, Specchia G, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013;368:22-33.
Tefferi A, Vardiman JW. Classification and diagnosis of myeloproliferative neoplasms: The 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia. 2008;22(1):14-22.
Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391-2405.
Barbui T, Barosi G, Birgegard G, et al. Philadelphia-negative classical myeloproliferative neoplasms: critical concepts and management recommendations from European LeukemiaNet. J Clin Oncol. 2011;29(6):761-770.
Keywords:
Polycythemia Vera, polycythemia vera symptoms, polycythemia vera treatment, polycythemia vera diagnosis, polycythemia vera icd 10, polycythemia vera lab values, polycythemia vera causes, polycythemia vera prognosis, polycythemia vera cancer, polycythemia vera test, polycythemia vera labs, polycythemia vera symptoms itching, polycythemia vera treatment medication, polycythemia vera treatment hydroxyurea, polycythemia vera treatment uptodate, polycythemia vera diagnosis age, jak2 mutation polycythemia vera, post polycythemia vera myelofibrosis, post polycythemia vera leukemia.






Was wondering if having primary PCV can contribute to bone weakening ? I had a seizure in March and found out later that I had some compression fractures in my spine. I had no other trauma. I’ve been in pain since March but the fractures, from what one spine specialist told me, aren’t large enough to be treated. I’m awaiting a new CT scan to see if the fractures have gotten better or worse since my July scan.
Will any change in diet help my weakened bones ?
Thanks
Hi Maryann,
Thank you for your comment.
First, do you have osteoporosis?
I don’t know how old are you, but if you are older than fifty I would recommend DEXA scan.
It would be also helpful to check your ESR, myeloma screen and Vitamin D blood levels.
I don’t think there is a direct link between PRV and the compression fractures in your spine!
If you are vitamin D deficient you might benefit from some oral vitamin D and Calcium supplements.
Best wishes,
Author
Hello. are labs showing WBC: 10.3, RBC: 5.53, Hemoglobin: 16.1, Hematocrit 49.4, Platelets: 342, Neutrophils: 7.6 Basophils: 0, Eosinophils: .2, Lymphocytes 1.9, Monocytes: .7 indicitive of PVR or any other blood cancer or serious condition? Thank you. – Chris
Also, do these numbers only go up with PV and similar blood cancers, and would you see an increase in values over 70 days?
Hi Chris,
Thanks for your comment.
The figures you mentioned are likely those of 2ry polycythaemia, not primary polycythaemia (PRV).
If you smoke or have a lung disease or are dehydrated that may explain your mild polycythemia.
Give up smoking if you smoke and maintain adequate hydration and repeat your CBC after 8 weeks.
BW,
Hello. Thank you so much for responding. If I may, there is a little more to the story and I would greatly appreciate your further thoughts in case your opinion changes. I had 3 labs done starting 70 days ago for a physical. I am a 48 year old male.
The first lab showed (SEPT 4):
WBC: 10.32, RBC: 5.76, Hemoglobin: 17, Hematocrit: 50.3, Netrophils: 74.6.
we repeated the labs 3 weeks later because I am a very nervous patient (SEPT 20):
WBC: 11.7, RBC: 5.52, Hemoglobin: 16.6, Hematocrit: 49.7, Neutrophils: 9.0
We then waited about two months and repeated the labs again and got the numbers I shared with you in my original post (NOV 17):
WBC: 10.3, RBC: 5.53, Hemoglobin: 16.1, Hematocrit: 49.3, Neutrophils: 7.6.
I am a very nervous individual and patient, so thinking about this does cause me daily stress. I do not smoke and do not live at a high altitude ( Michigan ). The good news is the numbers do seem stable or going down after close to 3 months from the initial lab work. But they are still elevated. I have had a very stressful year, losing both my parents and dealing with their house, so I have had some fatigue and perhaps some blurry vision in my right eye, but those may or may not be connected. Dehydration might factor, as it is possible I hadn’t been consuming as much water as I should. Thanks again for your incite and time. Best – Chris
Hi Chris,
Thanks for the update.
As per my previous reply, your mild polycythemia is likely reactive/relative and you should rest assured.
However, if you would like an additional piece of investigation to do in view of your anxiety, I would suggest checking your blood for the JAK2 mutation. If negative (as expected) you would just need to keep yourself well hydrated.
BW,
Sorry the neutrophils in the first lab ( SEPT 4) were 74.6%, or 7.71. Just to clarify.
Also, sorry for the third post, but forgot to include these values.
test 1, platelets: 354, test 2, platelets: 368, test 3, platelets: 342.
Thanks so much for your reply, that is reassuring. One last and quick question, would 70 days between the first and latest CBC panel generally be enough time to see a trend upward in the values? Thanks again, and I do see a hematologist on Monday.. As you have already detected, I am nervous and this weighs on me.
Hello, thank you for your advise. I did pursue a JAK12 test after talking to my doctor and it was negative, at least V617F. My spleen was also normal upon ultrasound. Thanks again, and I hope this fairly confidently rules out PRV.
Hello. Thank you again for you time. I did get one more test back and I was still a bit concerned. I had my erythropoietin tested and my value was 5. I know from Google that lower values are associated with primary Polycythemia, not secondary.
Even though I had a normal spleen reading and my JAK2V617F was negative,do I need to further test for what they call Exon 12 and 14 mutations? What are the chances I have PVR given my value of Erythropoietin, in your opinion?
As always, I appreciate your thoughts and your time.