Malignant Infiltration of Bone Marrow
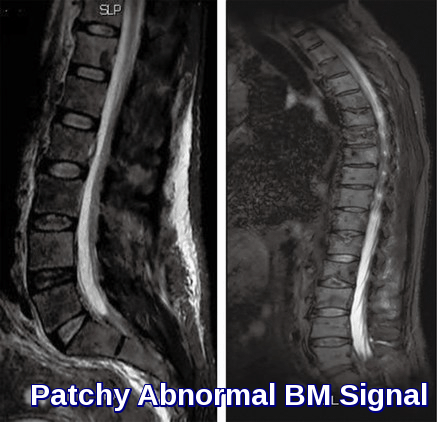
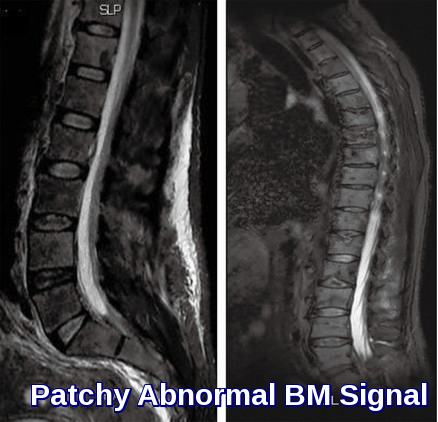
Patchy abnormal bone marrow signal on MRI demonstrating heterogeneous marrow infiltration, a key imaging feature in malignant bone marrow infiltration.
Malignant infiltration of the bone marrow is a significant clinical finding that occurs when solid tumors or hematologic malignancies spread to the marrow space, disrupting normal hematopoiesis. In adults, this process most frequently results from metastatic carcinomas—particularly those originating in the prostate, breast, and lung—although any cancer capable of hematogenous dissemination, including tumors of the colon and thyroid, may involve the marrow. In children, bone marrow infiltration is most commonly associated with aggressive solid tumors such as neuroblastoma, rhabdomyosarcoma, Ewing’s sarcoma, and retinoblastoma. Understanding the typical tumor types, patterns of spread, and clinical implications is essential for early detection and optimal management.
The bone marrow is a frequent site of involvement for tumors that spread hematogenously, making it a critical reservoir for metastatic disease. Disseminated tumor cells originating from primary solid cancers can seed the marrow, contributing to disease progression, relapse, and poor outcomes. Identifying these cells plays a crucial role in accurate staging, prognostication, and guiding decisions regarding systemic and adjuvant therapy.

Leukoerythroblastic blood picture demonstrating nucleated red blood cells, circulating myelocytes, and tear drop RBCs—classic peripheral smear findings in malignant bone marrow infiltration.
In malignant infiltration of bone marrow, the blood count may be normal although pancytopenia may occur and there may be leukoerythroblastic blood picture. Malignant infiltration of bone marrow by the metastatic tumor may be focal or diffuse.
Bone marrow aspirates and trephine biopsies are sensitive techniques for detecting bone marrow infiltration. Marrow aspirates may be difficult because of fibrosis and trephine biopsies should also be performed.
Reticulin and collagen fibrosis are commonly present and are most marked in those cases with greater degrees of marrow infiltration. Marked fibrosis is most common in carcinomas of the breast, stomach, prostate, and lung.
Trephine biopsy is more sensitive than bone marrow aspiration and sensitivity is increased
by performing bilateral biopsies or by obtaining a single large biopsy and therefore these two procedures should be regarded as complementary. The two primary sites whose identification is most important because of their sensitivity to hormonal therapy are breast and prostate.
The detection of tumor cells in a trephine biopsy when none are demonstrable in smears of aspirate is not uncommon. However, occasionally tumor cells are seen in aspirate smears when trephine biopsy is normal.
The features of cancer cells include:
- A tendency to form clumps.
- High nuclear to cytoplasmic ratio.
- Nuclear moulding.
- Large prominent nucleoli.
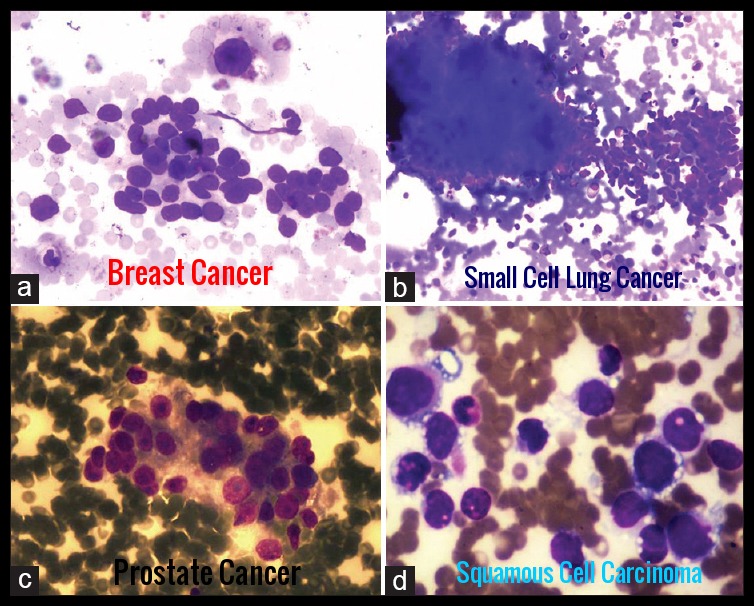
Bone marrow aspirate demonstrating malignant infiltration by various solid tumors—including breast cancer, small cell lung cancer, prostate cancer, and squamous cell carcinoma—highlighting the diverse cytologic patterns seen in metastatic bone marrow involvement.
Histology:
Some tumors can be clearly identified by cytochemistry. Adenocarcinoma cells, for instance, may stain with mucin stains.
Histologic section demonstrating metastatic colon adenocarcinoma infiltrating bone, a characteristic pattern of malignant bone marrow and skeletal involvement in advanced colorectal cancer.
Other tumors can be very difficult to differentiate from hematological malignancies and cell marker studies may then be useful. The CD45 antigen is expressed on most hematological tumors but not other cancers.
Radiology:
The presence of lytic and blastic lesions on skeletal radiographic films is common in patients with prostate, lung, or breast cancer metastases.
Bone scans are sensitive for detecting bone metastases, while magnetic resonance imaging (MRI) scans of the involved area can detect marrow infiltration.

MRI spine demonstrating heterogeneous marrow signal throughout the vertebral column, a classic radiologic feature of diffuse bone marrow infiltration in multiple myeloma.
MRI can detect intramedullary infiltration in a highly advanced manner. It is also useful for the detection of tumor extension, associated soft tissue masses, and neurological compromise. MRI can increase the rate of successful bone marrow biopsies as it can assess a large volume of bone marrow noninvasively and relatively quickly.
Treatment:
Management focuses on treating the underlying malignancy driving the bone marrow infiltration and providing targeted supportive care. Patients may require transfusions, infection prophylaxis, analgesia, and rapid correction of severe cytopenias. When vertebral involvement causes neurological symptoms or imaging shows impending spinal cord compression (SCC), urgent intervention is essential. High-dose corticosteroids, prompt MRI assessment, and early referral for radiotherapy or surgical decompression are crucial to prevent irreversible neurological deficits.
Prognosis:
Prognosis in malignant marrow infiltration depends on the primary tumor, disease burden, and severity of cytopenias. The development of spinal cord compression significantly worsens outcomes and requires immediate treatment to preserve motor and sensory function. A leukoerythroblastic blood picture reflects advanced disease and may correlate with a poorer short-term prognosis. Patients with profound cytopenias are at increased risk of infection, bleeding, and rapid clinical decline, reinforcing the need for early detection and comprehensive oncologic management.
Questions and Answers:
What are the earliest signs of malignant bone marrow infiltration?
Early features often include unexplained anemia, thrombocytopenia, neutropenia, bone pain, back pain, recurrent infections, and fatigue. Peripheral smear findings such as tear drop cells, nucleated red cells, and myelocytes (a leukoerythroblastic picture) are strong clues to underlying marrow infiltration.
What cancers most commonly infiltrate the bone marrow?
In adults, breast cancer, prostate cancer, and lung cancer are the most frequent causes. Others include gastrointestinal cancers (especially colon cancer), thyroid cancer, melanoma, and neuroendocrine tumors. In children, neuroblastoma, rhabdomyosarcoma, Ewing’s sarcoma, and retinoblastoma are typical causes.
What are the key laboratory findings that suggest malignant marrow infiltration?
Characteristic findings include anemia, thrombocytopenia, leukopenia or pancytopenia, elevated LDH, high alkaline phosphatase, and a leukoerythroblastic blood film. The presence of tear drop cells, NRBCs, and early granulocytic precursors strongly supports the diagnosis.
How is malignant bone marrow infiltration diagnosed?
Diagnosis relies on bone marrow aspiration and trephine biopsy, often supported by MRI when diffuse or patchy marrow abnormalities are suspected. Cytology, immunohistochemistry, and cytogenetics help classify the underlying malignancy and guide treatment.
Does malignant bone marrow infiltration increase the risk of spinal cord compression?
Yes. Vertebral metastases associated with marrow infiltration can weaken the spine and lead to spinal cord compression. Red flags include severe back pain, radicular pain, limb weakness, sensory changes, and bladder or bowel dysfunction. Urgent MRI and immediate treatment with corticosteroids, radiotherapy, or surgical decompression are essential.
Is a leukoerythroblastic blood picture always a sign of advanced disease?
A leukoerythroblastic smear often indicates extensive marrow stress or replacement. In malignant infiltration, it frequently correlates with advanced disease burden and may be associated with a poorer short-term prognosis, especially when accompanied by severe cytopenias.
What supportive treatments are recommended for patients with malignant marrow infiltration?
Supportive care may include blood and platelet transfusions, broad-spectrum antibiotics, antifungals, growth factors, pain control, and management of metabolic complications. Definitive therapy targets the primary cancer through chemotherapy, hormonal therapy, targeted therapy, radiotherapy, or immunotherapy depending on tumor type.
References:
Brodchammer WL Jr, Keeling MM. The bone marrow biopsy, osteoscan, and peripheral blood in non-hematopoietic cancer. Cancer. 1977;40(2):836–840.
Delsol G, Guiu-Godfrin B, Guiu M, Pris J, Corberand J, Fabre J. Leukoerythroblastosis and cancer: frequency, prognosis, and physiopathologic significance. Cancer. 1979;44(3):1009–1013.
Kaur G, Basu S, Kaur P, Sood T. Metastatic bone marrow tumors: study of nine cases and review of the literature. J Blood Disord Transfus. 2011;2:110. doi:10.4172/2155-9864.1000110.
Besa EC. Myelophthisic Anemia: Background, Etiology, Epidemiology, Prognosis, and Management. Medscape Reference. Updated 2015. Available at: emedicine.medscape.com/article/204647-overview. Accessed November 2015.
Makoni SN, Laber DA. Clinical spectrum of myelophthisis in cancer patients. Am J Hematol. 2004;76(1):92–93.
Mellors RC. Biological characteristics of benign and malignant neoplasms. In: MedPath – Neoplasia. Available at: medpath.info/MainContent/Neoplasia/Neoplasia_02.html.
Anner RM, Drewinko B. Frequency and significance of bone marrow involvement by metastatic solid tumors. Cancer. 1977;39(3):1337–1344.
Savage RA, Hoffman GC, Shaker K. Diagnostic problems in detection of metastatic neoplasms by bone marrow aspirate compared with needle biopsy. Am J Clin Pathol. 1978;70(4):623–627.
Tefferi A, Hanson CA, Inwards DJ. How to interpret and pursue an abnormal complete blood cell count in adults. Mayo Clin Proc. 2005;80(7):923–936. (Useful for linking leukoerythroblastic pictures, cytopenias, and marrow infiltration.)
Jain P, Kumar L, Malhotra P, Gupta R, Pati HP. Bone marrow metastasis in solid tumors: a study of 54 cases. Indian J Pathol Microbiol. 2007;50(2):303–308.
Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–2405. (Provides modern context for marrow pathology and differential diagnoses when a leukoerythroblastic picture is seen.)
Bain BJ. Bone marrow trephine biopsy. J Clin Pathol. 2001;54(10):737–742. (Authoritative discussion of biopsy value in detecting metastatic marrow infiltration.)
Keywords:
malignant bone marrow infiltration, bone marrow infiltration cancer, myelophthisic anemia, metastatic bone marrow involvement, leukoerythroblastic blood picture, nucleated red blood cells smear, tear drop red blood cells, NRBCs peripheral smear, marrow infiltration MRI findings, patchy marrow signal MRI, diffuse marrow infiltration multiple myeloma, bone metastasis colon cancer histology, metastatic prostate cancer bone marrow, metastatic breast cancer bone marrow, metastatic lung cancer marrow, spinal cord compression cancer, malignant spinal cord compression symptoms, MRI spine marrow infiltration, bone marrow biopsy metastatic cancer, bone marrow metastasis diagnosis, marrow metastases prognosis, cytopenias malignancy, pancytopenia cancer causes, anemia due to marrow infiltration, thrombocytopenia malignant infiltration, metastatic solid tumors bone marrow, neuroblastoma marrow infiltration, rhabdomyosarcoma marrow involvement, Ewing sarcoma marrow metastasis, retinoblastoma marrow spread, cancer back pain red flags, hematology evaluation of cytopenias, trephine biopsy metastatic cancer, Ask Hematologist, Dr Moustafa Abdou





Please what is the life span of a patient with a infiltration of malignant cell in bone marrow
Hi Cecilia,
I presume you are talking here about cancer spreading from an organ like the lung, breast, prostate, etc to the bone rather than cancers which originate from the bone marrow itself like leukemia/lymphoma/myeloma. The spine is the most common location of metastatic disease.
In general, patient survival is dramatically shortened once skeletal spread (metastases) are present.
For example, the 5-year overall survival rate for people with prostate cancer is 93%, but once skeletal metastases are present, the average survival time is only 29 months.
However, patients are surviving and remaining active for longer periods as treatment protocols improve.
Most patients with metastatic bone disease survive for 6-48 months.
Patients with breast and prostate carcinoma live longer than those with lung carcinoma.
Patients with renal cell or thyroid carcinoma have a variable life expectancy.
As the treatment protocols keep improving survival in turn improves.
You can read more about the prognosis and outcome of metastatic bone disease through this link.
Best wishes,
Thanks sir..May I ask about the expected marrow findings in patients with solid malignancies other than myelophthsis or fibrosis….The need for Immunohistochemistry(CD45,Cytokeratin )if the primary solid malignancy is already known..Finally ,The role of PET CT
Hi Sabry,
Thank you for your comment.
Certain solid tumors such as lung, breast, and prostate have the ability to spread to the bone marrow, resulting in the infiltration of tumor cells. This infiltration can manifest as either focal or diffuse, and it has the potential to impact normal hematopoietic cells, leading to conditions such as anemia, thrombocytopenia, and leukopenia.
In cases where the primary solid tumor is suspected, the diagnosis often necessitates bone marrow aspiration and biopsy for morphological evaluation, immunohistochemistry, and molecular studies.
Best regards,
Dr. M Abdou