Leishmaniasis
Leishmaniasis is a disease caused by an intracellular protozoan parasite (genus Leishmania) transmitted by the bite of a sand fly. The disease is present in scattered areas worldwide. Human infection is caused by 20 Leishmania species that are morphologically indistinguishable but can be differentiated by laboratory analysis. Leishmania promastigotes are transmitted by sand flies to vertebrate hosts.
The clinical spectrum of leishmaniasis ranges from a self-resolving cutaneous ulcer to a mutilating mucocutaneous disease and even to lethal systemic illness. Therapy has long been a challenge in the more severe forms of the disease, and it is made more difficult by the emergence of drug resistance.
Pathophysiology:
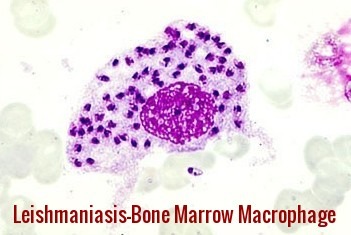
After inoculation by a sandfly, promastigotes are phagocytized by host macrophages; inside these cells, they transform into amastigotes.
The parasites may remain localized in the skin or spread to internal organs or the mucosa of the nasopharynx, resulting in 3 major clinical forms of leishmaniasis:
- Cutaneous
- Mucosal
- Visceral
Clinical features:
Cutaneous Leishmaniasis:
In cutaneous leishmaniasis, a well-demarcated skin lesion develops at the site of a sandfly bite, usually within several weeks to months. Multiple lesions may occur after multiple infective bites or with metastatic spread. Their appearance varies.
The initial lesion is often a papule that slowly enlarges, ulcerates centrally, and develops a raised, erythematous border where intracellular parasites are concentrated. Ulcers are typically painless and cause no systemic symptoms unless secondarily infected. Lesions usually heal spontaneously after several months but may persist for years. They leave a depressed, burn-like scar. The course depends on the infecting Leishmania species and the host’s immune status.
Mucocutaneous Leishmaniasis:
Mucocutaneous leishmaniasis consists of the relentless destruction of the oropharynx and nose, resulting in extensive midfacial destruction. The disease starts with a primary cutaneous ulcer. This lesion heals spontaneously, but progressive mucosal lesions develop months to years later. Typically, patients have nasal stuffiness, discharge, and pain. Over time, the infection may progress, resulting in gross mutilation of the nose, palate, or face.
Visceral Leishmaniasis:
In visceral leishmaniasis (kala-azar), the clinical manifestations usually develop gradually over weeks to months after inoculation of the parasite but can be acute. Irregular fever, hepatosplenomegaly, pancytopenia, and polyclonal hypergammaglobulinemia with a reversed albumin:globulin ratio occur. In some patients, there are twice-daily temperature spikes. Cutaneous skin lesions rarely occur. Emaciation and death occur within months to years in patients with progressive infections. Those with asymptomatic, self-resolving infections and survivors (after successful treatment) are resistant to further attacks unless cell-mediated immunity is impaired (eg, by AIDS). Relapse may occur years after the initial infection.
Post kala-azar dermal leishmaniasis:
Post kala-azar dermal leishmaniasis (PKDL) develops months to years after the patient’s recovery from visceral leishmaniasis, with cutaneous lesions ranging from hypopigmented macules to erythematous papules and from nodules to plaques; the lesions may be numerous and persist for decades. PKDL lesions are thought to be a reservoir for the spread of infection in endemic countries.
Diagnosis:
- A definite diagnosis is made by demonstrating organisms in Giemsa-stained smears, by isolating Leishmania in cultures, or by PCR-based assays of aspirates from the spleen, bone marrow, liver, or lymph nodes in patients with visceral leishmaniasis or of biopsy, aspirates, or touch preparations from a skin lesion. Parasites are usually difficult to find or isolate in biopsies of mucosal lesions.
- Serologic tests can help diagnose visceral leishmaniasis; high titers of antibodies to a recombinant leishmanial antigen (rk39) are present in most immunocompetent patients with visceral leishmaniasis. Antibodies may be absent in patients with AIDS or other immunocompromising conditions. Serologic tests for antileishmanial antibodies are not helpful in the diagnosis of cutaneous leishmaniasis.
- The leishmanin skin test is not available in the US. It is typically positive in patients with cutaneous and mucosal leishmaniasis but negative in those with active visceral leishmaniasis.
Prevention and Control:
No vaccines or drugs to prevent infection are available. The best way for travelers to prevent infection is to protect themselves from sand fly bites.
Avoid outdoor activities, especially from dusk to dawn, when sand flies generally are the most active.
When outdoors (or in unprotected quarters):
- Minimize the amount of exposed (uncovered) skin. To the extent that is tolerable in the climate, wear long-sleeved shirts, long pants, and socks; and tuck your shirt into your pants.
- Apply insect repellent to exposed skin and under the ends of sleeves and pant legs. The most effective repellents generally are those that contain the chemical DEET (N,N-diethylmetatoluamide).
When indoors:
- Stay in well-screened or air-conditioned areas.
- Keep in mind that sand flies are much smaller than mosquitoes and therefore can get through smaller holes.
- Spray living/sleeping areas with an insecticide to kill insects.
- If you are not sleeping in a well-screened or air-conditioned area, use a bed net and tuck it under your mattress. If possible, use a bed net that has been soaked in or sprayed with a pyrethroid-containing insecticide. The same treatment can be applied to screens, curtains, sheets, and clothing (clothing should be retreated after five washings).
Treatment:
The treatment is determined by where the disease is acquired, the species of Leishmania, and the type of infection.
For visceral leishmaniasis in India, South America, and the Mediterranean, liposomal amphotericin B is the recommended treatment and is often used as a single dose. Rates of cure with a single dose of amphotericin have been reported as 95%.
In India, almost all infections are resistant to pentavalent antimonials.
In Africa, a combination of pentavalent antimonials and paromomycin is recommended. These, however, can have significant side effects.
Miltefosine, an oral medication, is effective against both visceral and cutaneous leishmaniasis. Side effects are generally mild, though it can cause birth defects if taken early in pregnancy.
Cutaneous ulcers will often heal without treatment. However, treatment can speed healing and reduce scarring. It can also prevent the development of further disease. Ulcers on the face that cause disfigurement may require plastic surgery.
A number of topical treatments may be used for cutaneous lesions e.g. topical paromomycin.
References:
World Health Organization. Leishmaniasis: the disease and its epidemiology. Available at http://www.who.int/leishmaniasis/disease_epidemiology/en/. Accessed: April 10, 2014.
Centers for Disease Control and Prevention. Parasites home: leishmaniasis. Epidemiology & risk factors. Available at http://www.cdc.gov/parasites/leishmaniasis/epi.html. Accessed: April 11, 2014.
McHugh CP, Melby PC, LaFon SG. Leishmaniasis in Texas: epidemiology and clinical aspects of human cases. Am J Trop Med Hyg. 1996 Nov. 55(5):547-55.
CDC – Leishmaniasis – Prevention & Control. https://www.cdc.gov/parasites/leishmaniasis/prevent.html
Eradication of Leishmaniasis from Yemen Project (ELYP) Regional Leishmaniasis Control Center (RLCC), Yemen. https://rlccye.blogspot.com/2015/11/leishmaniasis-in-yemen.html














I cannot believe it. I had this from River Maya in Mexico, it developed several weeks after I returned. I was on a cocktail of antibiotics and creams which did nothing. I am left with scarring on my back, nose and face. It took a year to stop spreading and is now finally getting better18 months on.
I will have to see my gp now to let them know what it was and see if I need treatment.
Hi Ross,
Thank you for sharing your experience with us.
Best wishes,
Would you be interested to do a tour with me in the US?
The people of the world need to learn….physicians need to learn.
Thank you