Coronavirus and Blood
Coronavirus and Blood:
Does coronavirus have direct effects on Blood?
The United States and countries around the world face a major public health concern with the current outbreak of the novel (new) coronavirus (COVID-19). The emergence of the novel coronavirus outbreak in December 2019 was followed by its spread on a global scale unparalleled in the last 100 years. At present, it has claimed over 740,000 lives the world over, with over 20 million cases have tested positive.
Coronavirus symptoms include a dry cough, shortness of breath, and in severe cases, respiratory failure and death.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) sequence was first uploaded in early 2020, but as of now, over 17,000 genomes have been sequenced from viral strains isolated all over the world. This allows for rapid RNA screening in human tissues as well as environmental samples.

Novel Coronavirus SARS-CoV-2: This scanning electron microscope image shows SARS-CoV-2 (round gold objects) emerging from the surface of cells cultured in the lab. SARS-CoV-2, also known as 2019-nCoV, is the virus that causes COVID-19. The virus shown was isolated from a patient in the U.S. Credit: NIAID-RML.
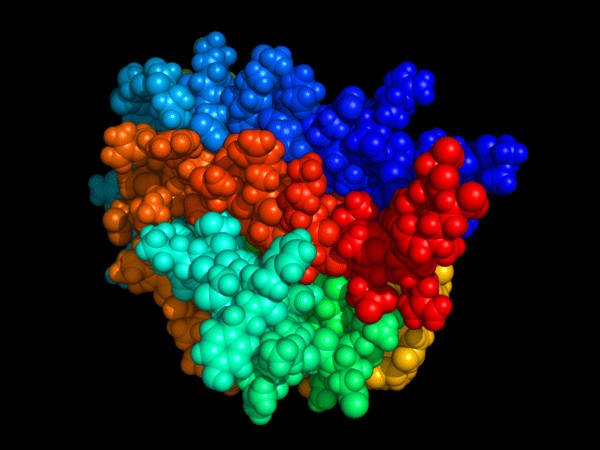
Researchers in the U.S. have shown that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may alter key protein structures on red blood cells (RBCs) and compromise the transport and delivery of oxygen in patients with coronavirus disease 2019 (COVID-19).
Altered protein-membrane homeostasis may contribute to clot formation and the coagulation complications that are sometimes observed in severely ill patients, say Steven Spitalnik (Columbia University, New York) and colleagues.
Susceptibility of RBCs to SARS-CoV-2:
The causative agent – SARS-CoV-2 – infects cells by using its Spike protein to bind host angiotensin-converting enzyme 2 (ACE2) and fuse with the cell membrane. This ACE2 receptor is abundantly expressed on lung alveolar epithelial cells.
According to Spitalnik and colleagues, proteomics studies have previously identified angiotensin and ACE2-interacting proteins on the surface of RBCs, suggesting that these cells may be susceptible to SARS-CoV-2 invasion.
Since RBCs are responsible for transporting oxygen around the body, their alteration may contribute to the severity of hypoxemia among patients with severe COVID19, suggests the team.
Because RBCs are critical for oxygen transport and off-loading, the severely low oxygen saturations seen in critically ill COVID-19 patients suggest the importance of determining whether SARS-CoV-2 infection directly or indirectly affects RBC metabolism to influence their gas transport, structural integrity, and circulation in the bloodstream,” they write.
Other hematological findings in SARS patients:
Severe acute respiratory syndrome (SARS) has recently recognized as a new human infectious disease. A novel coronavirus was identified as the causative agent of SARS. This report summarizes the hematological findings in SARS patients and proposes a hypothesis for the pathophysiology of SARS coronavirus related abnormal hematopoiesis.
Hematological changes in patients with SARS were common and included lymphopenia (68% – 90% of adults; 100% of children, n = 10), thrombocytopenia (20% – 45% of adults, 50% of children), and leukopenia (20% – 34% of adults, 70% of children). The possible mechanisms of this coronavirus on the blood system may include (1) directly infect blood cells and bone marrow stromal cells via CD13 or CD66a; and/or (2) induce autoantibodies and immune complexes to damage these cells. In addition, lung damage in SARS patients may also play a role in inducing thrombocytopenia by (1) increasing the consumption of platelets/megakaryocytes; and/or (2) reducing the production of platelets in the lungs. Since the most common hematological changes in SARS patients were lymphopenia and immunodeficiency, it is postulated that hematopoietic growth factors such as G-CSF, by mobilizing endogenous blood stem cells and endogenous cytokines, could become a hematological treatment for SARS patients, which may enhance the immune system against these viruses.
Detection of Virus in Human Blood or Blood Cells:
A recent study by researchers in Cairo, Egypt, and published on the preprint server medRxiv was designed to test for the presence of the virus in human blood or any blood cells, which could allow the virus to hide from the immune system or to be trafficked to other organs. It is especially relevant given some (doubtful) reports that the virus could infect lymphocytes.
Other scientists have claimed that the virus perhaps attacks hemoglobin, or that it is to be found in the blood of infected patients, or the peripheral blood mononuclear cells (PBMCs), as is the case with other infectious viruses like hepatitis B, hepatitis C or HIV.
The current study, therefore, used computational analysis on three genome sequences from PBMCs from active COVID-19 patients, three from healthy donor PBMCs, and two from bronchoalveolar lavage fluid (BAL) from patients. They found that traces and large amounts of SARS-CoV-2 RNA were found in PBMCs and BAL, respectively.
The results showed that the BAL and PBMC samples were widely separated, as expected, while the PBMCs from healthy and patient samples were slightly separated for the most part. Viral RNA was present in all the BALF sequences at 2.15% of the total reads (median). The PBMC of one patient also showed two reads that matched the SAR-CoV-2 protein and surface glycoprotein.
Though the amount of viral RNA is small, it is undoubtedly that of the SARS-CoV-2. One of the reads encodes a polyprotein, which takes part in viral transcription and replication, and which is the largest of the coronavirus proteins. Another encoded the spike protein, which is responsible for the viral entry into human cells that carry the ACE2 molecule receptor.
Coronavirus and Pulmonary Embolism (PE):
Frequently Asked Questions
How do we diagnose PE if we cannot perform CTPA or V/Q lung scan because the patient must remain in isolation (e.g. due to risk of virus aerosolization, lack of PPE) or is too unstable?
When objective imaging is not feasible to confirm or refute a diagnosis of PE, clinicians must rely on clinical assessment based on history, physical findings, and other tests. Very limited observational data suggest that up to 15-39% of patients with COVID-19 infection who require mechanical ventilation have acute PE/DVT. The likelihood of PE is moderate to high in those with signs or symptoms of DVT, unexplained hypotension or tachycardia, unexplained worsening respiratory status, or traditional risk factors for thrombosis (e.g., history of thrombosis, cancer, hormonal therapy). If feasible, consider doing bilateral compression ultrasonography (CUS) of the legs, echocardiography, or point-of-care ultrasonography (POCUS). These tests can confirm thrombosis if proximal DVT is documented on CUS or if a clot-in-transit is visualized in the main pulmonary arteries on echocardiography or POCUS, but they cannot rule out thrombosis if a clot is not detected.
Data suggested an increased PE prevalence in COVID-19 patients attending ED with an elevated D-dimer, and patients with levels >5000 ng/ml might benefit from CTPA to exclude concomitant PE.
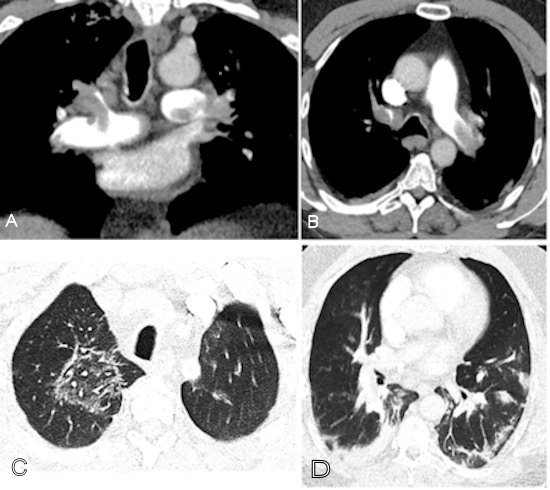
A COVID-19-positive patient with bilateral pulmonary emboli had D-dimer of > 10,000. A: Coronal CTPA image identifies bilateral pulmonary emboli that involve the left main pulmonary artery, distal right main pulmonary artery, right upper lobe pulmonary artery, and proximal segmental vessels. B: On an axial CPTA image, there is an embolus present in the left main and right upper lobe pulmonary arteries extending into the bilateral anterior segmental artery. C: A ground-glass opacity is present in the right upper lobe centrally with a reversed halo appearance, peripheral dense area, and central ground-glass opacity attributed to lung involvement from COVID-19. D: Axial image through the lung base demonstrates basilar consolidation compatible with COVID-19. Images and caption courtesy of the RSNA.
Does a normal D-dimer level effectively rule out PE/DVT?
Yes. The value of D-dimer testing is the ability to rule out PE/DVT when the level is normal. Although the false-negative rate of D-dimer testing (i.e., PE/DVT is present but the result is normal) is unknown in this population, low rates of 1 – 2% using highly sensitive D-dimer assays have been reported in other high-risk populations. Therefore, a normal D-dimer level provides reasonable confidence that PE/DVT is not present and anticoagulation should continue at a prophylactic dose rather than empiric therapeutic dosing. In addition, radiological imaging is not necessary when the D-dimer level is normal in the context of low pre-test probability.
N.B.
- Normally plasma is negative for D-dimer.
- Qualitative: It is negative
- Quantitative : < 250 ng/mL or < 250 µg/L ( SI unit)
- Critical value >40 mg/L (40 µg/mL).
Increased D-dimer levels are seen in:
Primary and secondary fibrinolysis:
-
- DIC
- Thrombolytic therapy.
- Deep vein thrombosis.
- Pulmonary embolism.
- Arterial thromboembolism.
- myocardial infarction.
- Vaso-occlusive crises of sickle cell anemia.
- Infection.
- Renal Failure.
- pregnancy ( Especially postpartum period).
- Malignancy.
- Surgery.
False-Positive D-Dimer Test:
- This is seen in heparin therapy.
- The Rheumatoid factor can give false high values of FDP.
- This test is positive in patients after surgery or trauma.
- The false-positive test is seen in estrogen therapy and pregnancy.
If D-dimer levels change from normal to abnormal or rapidly increase on serial monitoring, is this indicative of PE/DVT?
An elevated D-dimer level does not confirm a diagnosis of PE/DVT in a patient with COVID-19 because the elevated D-dimer may result from many other causes. If possible, CTPA and/or bilateral CUS should be performed to investigate for PE/DVT. It is important to determine if there are any new clinical findings that indicate acute PE/DVT and if there are other causes of high D-dimer levels, such as secondary infection, myocardial infarction, renal failure, or coagulopathy. Published data have shown that the majority of patients with progressive, severe COVID-19 infection with acute lung injury/ARDS have very high D-dimer and fibrinogen levels, supportive of a hypercoagulable state from cytokine storm syndrome.

COVID-19 – rapidly progressive acute respiratory distress syndrome. A 70-year old female patient admitted with acute respiratory failure, fever (38ºC), and dyspnoea. She was tachypnoeic (30 bpm), with lymphopenia and low oxygen saturation (SpO2 85%, PAFI<250).
What are the risks and benefits of empiric therapeutic anticoagulation in COVID-19 patients?
COVID-19 infection is associated with high morbidity and mortality largely due to respiratory failure, with microvascular pulmonary thrombosis perhaps playing an important pathophysiological role. Having undiagnosed or untreated PE may worsen patient outcomes. Anti-inflammatory effects of heparin/LMWH may offer benefit and anti-viral mechanisms have been demonstrated for factor Xa inhibitors in animal studies. Consequently, the use of empiric therapeutic anticoagulation in certain COVID patients who do not have PE/DVT has been advocated. However, this remains controversial because the true incidence of PE/DVT in patients receiving pharmacological thromboprophylaxis remains uncertain and data to show improved outcomes with therapeutic anticoagulation are lacking. Current clinical trials addressing this question are underway. The risk of major bleeding is also heightened in those with risk factors for bleeding, such as older age, liver or renal impairment, and previous history of bleeding. Objective imaging to confirm a diagnosis of PE/DVT should, if possible, be done prior to starting therapeutic anticoagulation.
Are there any clinical scenarios in which empiric therapeutic anticoagulation would be considered in COVID-19 patients?
In cases where there are no contraindications for therapeutic anticoagulation and there is no possibility of performing imaging studies to diagnose PE or DVT, empiric anticoagulation has been proposed in the following scenarios:
- Intubated patients who develop sudden clinical and laboratory findings highly consistent with PE, such as desaturation, tachycardia, increased CVP or PA wedge pressure, or evidence of right heart strain on echocardiogram, especially when CXR and/or markers of inflammation are stable or improving.
- Patients with physical findings consistent with thrombosis, such as superficial thrombophlebitis, peripheral ischemia or cyanosis, thrombosis of dialysis filters, tubing or catheters, or retiform purpura (branching lesions caused by thrombosis in the dermal and subcutaneous vasculature).
- Patients with respiratory failure, particularly when D-dimer and/or fibrinogen levels are very high, in whom PE or microvascular thrombosis is highly suspected and other causes are not identified (e.g., ARDS, fluid overload).

Bilateral retiform purpura in both legs as a dermatological sign of coronavirus disease 2019 (COVID‐19) coagulopathy
If a patient is empirically started on anticoagulation for suspected PE, how long should they be anticoagulated? What if a later investigation shows no evidence of PE?
All patients with COVID-19 who are started on empiric therapeutic anticoagulation for presumed or documented PE should be given a minimum course of 3 months of the therapeutic regimen (provided the patient tolerates treatment without serious bleeding). Thrombus resolution can occur within a few days of effective anticoagulation, so negative results from delayed testing should not be interpreted as implying PE or DVT was not previously present. At 3 months, therapeutic anticoagulation can stop, provided the patient has recovered from COVID-19 and has no ongoing risk factors for thrombosis or other indications for anticoagulation (e.g. atrial fibrillation).
Protective Effect of Aspirin on Coronavirus Patients (PEAC):
COVID-19 has a high infection rate and mortality, and serious complications such as heart injury cannot be ignored. Cardiac dysfunction occurred in COVID-19 patients, but the law and mechanism of cardiac dysfunction remain unclear. The occurrence of progressive inflammatory factor storm and coagulation dysfunction in severe and fatal cases of novel coronavirus pneumonia (NCP) points out a new direction for reducing the incidence of severe and critically ill patients, shortening the length of duration in severe and critically ill patients and reducing the incidence of complications of cardiovascular diseases. Aspirin has the triple effects of inhibiting virus replication, anticoagulant, and anti-inflammatory, but it has not received attention in the treatment and prevention of NCP. Although Aspirin is not commonly used in the guidelines for the treatment of NCP, it was widely used in the treatment and prevention of a variety of human diseases after its first synthesis in 1898. Subsequently, aspirin has been confirmed to have an antiviral effect on multiple levels. Moreover, one study has confirmed that aspirin can inhibit virus replication by inhibiting prostaglandin E2 (PGE2) in macrophages and upregulation of type I interferon production. Subsequently, pharmacological studies have found that aspirin is an anti-inflammatory and analgesic drug by inhibiting cox-oxidase (COX). Under certain conditions, the platelet is the main contributor of an innate immune response, studies have found that in the lung injury model in dynamic neutrophil and platelet aggregation.
In summary, the early use of aspirin (100mg a day) in covid-19 patients, which has the effects of inhibiting virus replication, anti-platelet aggregation, anti-inflammatory, and anti-lung injury, is expected to reduce the incidence of severe and critical patients, shorten the length of hospital duration and reduce the incidence of cardiovascular complications.
Dexamethasone in patients with severe Coronavirus:
Patients with severe COVID-19 can develop a systemic inflammatory response that can lead to lung injury and multisystem organ dysfunction. It has been proposed that the potent anti-inflammatory effects of corticosteroids might prevent or mitigate these deleterious effects. The Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial, a multicenter, randomized, open-label trial in hospitalized patients with COVID-19, showed that the mortality rate was lower among patients who were randomized to receive dexamethasone than among those who received the standard of care. This benefit was observed in patients who required supplemental oxygen at enrollment. No benefit of dexamethasone was seen in patients who did not require supplemental oxygen at enrollment.
On the basis of the preliminary report from the RECOVERY trial, the COVID-19 Treatment Guidelines Panel recommends using dexamethasone 6 mg per day for up to 10 days or until hospital discharge, whichever comes first, for the treatment of COVID-19 in hospitalized patients who are mechanically ventilated (AI) and in hospitalized patients who require supplemental oxygen but who are not mechanically ventilated (BI).
The Panel recommends against using dexamethasone for the treatment of COVID-19 in patients who do not require supplemental oxygen (AI).
If dexamethasone is not available, the Panel recommends using alternative glucocorticoids such as prednisone, methylprednisolone, or hydrocortisone (AIII).
Covid vaccines and blood clots:
COVID-19 vaccines are medicines that prevent disease caused by the novel coronavirus SARS-CoV-2 by triggering an immune response.
Safe and effective vaccines for COVID-19 are needed because they protect individuals from becoming ill. This is particularly important for healthcare professionals and vulnerable populations such as older people, and those with underlying medical problems like cardiovascular disease, diabetes, chronic respiratory disease, and cancer.
The COVID-19 pandemic is a global crisis, with devastating health, social and economic impacts. COVID-19 can cause severe disease and death. It has unknown long-term consequences in people of all ages, including in otherwise healthy people.
The European Commission confirmed it had granted conditional marketing authorization for the COVID-19 Vaccine BioNTech and Pfizer, the COVID-19 Vaccine Moderna, the COVID-19 Vaccine AstraZeneca, and the COVID-19 Vaccine Janssen.
Misinformation about Covid vaccine risks and concerns over rare blood clots have had many searching the web for answers.
Public Health Wales: “Following reports of an extremely rare and specific blood clot after vaccination with the AstraZeneca Covid-19 vaccine, the Medicines and Healthcare Regulatory Agency (MHRA) and the Joint Committee on Vaccination and Immunisation (JCVI) confirmed that this type of blood clot with low platelets are a possible side effect of the vaccine. However, they continue to advise that the benefits of vaccination with the AstraZeneca Covid-19 vaccine continue to outweigh the risks of Covid-19 for the vast majority of adults.
The Centers for Disease Control and Prevention (CDC) and the U.S. Food and Drug Administration (FDA) recommended a pause in the use of the Johnson & Johnson/Janssen (J&J) COVID-19 vaccine while they investigated reports of a small number of women in the U.S. who developed a rare and severe type of blood clot within the two weeks following receipt of the J&J COVID-19 vaccine.
Jo Jerrome, chief executive of Thrombosis UK: “Having a previous thrombosis or thrombophilia (sticky blood) is not a risk factor for developing the rare post-Covid-19 vaccine thrombosis and thrombocytopenia.”
References:
Liji Thomas, MD. Does COVID-19 infect peripheral blood cells? https://www.news-medical.net/news/20200519/Does-COVID-19-infect-peripheral-blood-cells.aspx
Moustafa, A., and Aziz, R. K. (2020). Traces of SARS-CoV-2 RNA in the Blood of COVID-19 Patients. medRxiv preprint doi: https://doi.org/10.1101/2020.05.10.20097055. https://www.medrxiv.org/content/10.1101/2020.05.10.20097055v1
Sally Robertson, B.Sc. Blood cell damage in COVID-19 may compromise oxygen transport. https://www.news-medical.net/news/20200701/Blood-cell-damage-in-COVID-19-may-compromise-oxygen-transport.aspx
Spitalnik S, et al. Evidence for structural protein damage and membrane lipid remodeling in red blood cells from COVID-19 patients. bioRxiv 2020. doi: https://doi.org/10.1101/2020.06.29.20142703
Yang M, Hon KL, Li K, Fok TF, Li CK. The effect of SARS coronavirus on blood system: its clinical findings and the pathophysiologic hypothesis. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2003;11(3):217-221.
Vanessa C. L. Chong Kian Guan Eric Lim Bingwen Eugene Fan Stephrene S. W. Chan Kiat H. Ong Ponnudurai Kuperan. Reactive lymphocytes in patients with COVID‐19.
Agnes Lee, Maria deSancho, Menaka Pai, Menno Huisman, Stephan Moll, and Walter Ageno. COVID-19 and Pulmonary Embolism: Frequently Asked Questions.
Hematology.org https://www.hematology.org/covid-19/covid-19-and-pulmonary-embolism
Kate Madden Yee. Almost 40% of CTPA exams find PE in COVID-19 patients. https://www.auntminnie.com/index.aspx?sec=sup&sub=cto&pag=dis&ItemID=129487
D-Dimer test, Fragment D-dimer. https://www.labpedia.net/d-dimer-test-fragment-d-dimer/
Dr. Edgar Lorente. COVID-19 – rapidly progressive acute respiratory distress syndrome (ARDS). https://radiopaedia.org/cases/covid-19-rapidly-progressive-acute-respiratory-distress-syndrome-ards?lang=gb
X. Bosch‐Amate P. Giavedoni S. Podlipnik C. Andreu‐Febrer J. Sanz‐Beltran A. Garcia‐Herrera L. Alós J.M. Mascaró. Retiform purpura as a dermatological sign of coronavirus disease 2019 (COVID‐19) coagulopathy. https://onlinelibrary.wiley.com/doi/10.1111/jdv.16689
Novel Coronavirus (2019-nCoV) situation reports – World Health Organization (WHO)
2019 Novel Coronavirus (2019-nCoV) in the U.S. -. U.S. Centers for Disease Control and Prevention (CDC)
Protective Effect of Aspirin on COVID-19 Patients (PEAC). https://clinicaltrials.gov/ct2/show/NCT04365309
RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with COVID-19—preliminary report. N Engl J Med. 2020. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32678530.
Catherine Evans – BBC News. Covid vaccines and blood clots: Your questions answered https://www.bbc.com/news/uk-wales-56764182
Lisa Maragakis, M.D., and Gabor Kelen, M.D. Is the COVID-19 Vaccine Safe? https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/is-the-covid19-vaccine-safe
Perera A, Chowdary P, Johnson J, et al. A 10-fold and greater increase in D-dimer at admission in COVID-19 patients is highly predictive of pulmonary embolism in a retrospective cohort study. Therapeutic Advances in Hematology. January 2021. doi:10.1177/20406207211048364