Hemolytic Disease Of The Newborn (HDN)
Hemolytic disease of the newborn (HDN) used to be a major cause of fetal loss and death among newborn babies. The first description of HDN is thought to be in 1609 by a French midwife who delivered twins—one baby was swollen and died soon after birth, the other baby developed jaundice and died several days later. For the next 300 years, many similar cases were described in which newborns failed to survive.
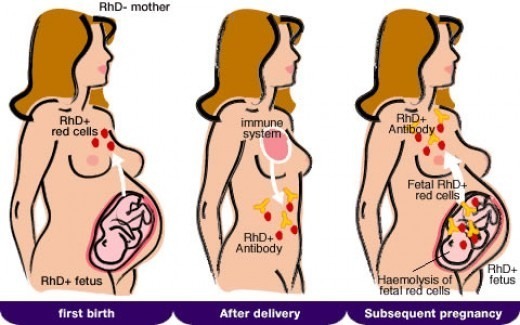
It was not until the 1950s that the underlying cause of HDN was clarified; namely, the newborn’s red blood cells (RBCs) are being attacked by antibodies from the mother. The attack begins while the baby is still in the womb and is caused by an incompatibility between the mother’s and baby’s blood.
By the 1960s, trials in the United States and the United Kingdom tested the use of therapeutic antibodies that could remove the antibodies that cause HDN from the mother’s circulation. The trials showed that giving therapeutic antibodies to women during their pregnancy largely prevented HDN from developing. By the 1970s, routine antenatal care included the screening of all expectant mothers to find those whose pregnancy may be at risk of HDN and giving preventative treatment accordingly. This has led to a dramatic decrease in the incidence of HDN, particularly severe cases that were responsible for stillbirth and neonatal death.
Antigen-negative mothers bearing an antigen-positive child are frequently immunized by fetal cells at birth. The number of fetal red cells that enter the maternal circulation can be estimated with the Kleihauer test.
In subsequent pregnancies with an antigen-positive fetus, IgG antibodies are formed which cross the placenta and cause hemolysis in the fetus. Most cases of immune HDN are due to antibodies to rhesus D antigen. Nearly 15% of births are to rhesus D-negative mothers with a D-positive father and 75% of these children will be D-positive.
Clinical features:
- There is anemia in the affected fetus or child associated with nucleated red blood cells (NRBCs) in the neonate’s blood.
- At birth, the child is not severely jaundiced because of the placental clearance system, but jaundice may worsen rapidly and produce kernicterus if not treated promptly.
- In its severest form, there is cardiac failure, hepatosplenomegaly, and intrauterine death (hydrops fetalis).
Diagnosis:
- The blood group of the mother is routinely assessed, and the father is also tested if the mother is D-negative. A previous history of pregnancies, previously affected infants, abortions and blood transfusions (possible sensitization) is essential.
- During the pregnancy Rh positive antibodies can be measured in the maternal serum, and bilirubin can be measured in the amniotic fluid to assess the severity of the hemolysis.
- At birth, the degree of anemia is the best guide to the severity. The blood film reveals increased nucleated RBCs, reticulocytosis, polychromasia, anisocytosis, spherocytes, and cell fragmentation. The reticulocyte count can be as high as 40% in patients without intrauterine intervention.
- Positive maternal indirect Coombs test.
- Positive neonatal direct Coombs test.
- Ultrasound – to detect organ enlargement or fluid buildup in the fetus.
Treatment:
- As a rule, serial maternal antibody titers are monitored until a critical titer of 1:32, which indicates that a high risk of fetal hydrops has been reached. At this point, the fetus requires very intense monitoring for signs of anemia and fetal hydrops.
- In severe cases, intrauterine transfusion must be given. Transfused cells must be compatible with the mother’s serum.
- Exchange transfusion may be required soon after birth to prevent kernicterus. Fresh blood should be used.
- Phototherapy may augment bilirubin breakdown and avoid the necessity of exchange transfusion in mild cases.
References:
Bowman JM. Hemolytic disease (erythroblastosis fetalis). Creasy RK, Resnik R. Maternal-fetal medicine. 4th edition. Philadelphia: WB Saunders; 1999. 736-767.
Fasano RM. Hemolytic disease of the fetus and newborn in the molecular era. Semin Fetal Neonatal Med. 2015 Nov 14.
Luchtman-Jones L, Schwartz AL, Wilson DB. The blood and hematopoietic system. Fanaroff AA, Martin RJ, eds. Neonatal-Perinatal Medicine-Diseases of the Fetus and Infant. 8th ed. St. Louis, Mo: Mosby; 2006. Vol 2: 1287-1356.
Hemolytic disease of the newborn – Blood Groups and Red Cell Antigens – NCBI Bookshelf https://www.ncbi.nlm.nih.gov/books/NBK2266/
Urbaniak SJ, Greiss MA. RhD haemolytic disease of the fetus and the newborn. Blood Rev. 2000;14:44–61.
Keywords:
hemolytic disease of the newborn (hdn), hemolytic disease of the newborn (abo), hemolytic disease of the newborn (anti-kell), Hemolytic disease of the newborn (anti-RhE), hemolytic disease of the newborn diagnosis, hemolytic disease of the newborn rh, hemolytic disease of the newborn symptoms, hemolytic disease of the newborn treatment.









That was a great post. You did cover many aspects very precisely. I am glad that I came across the post.