Cold Agglutinin Disease
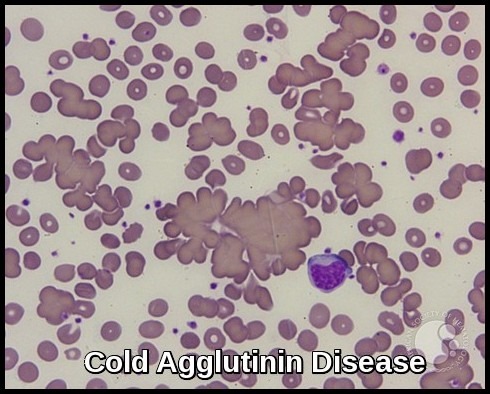
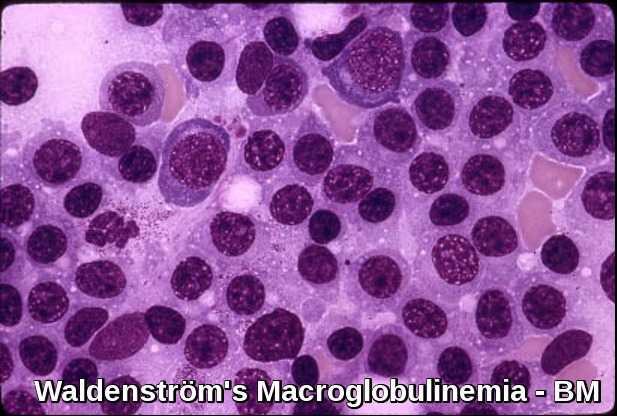
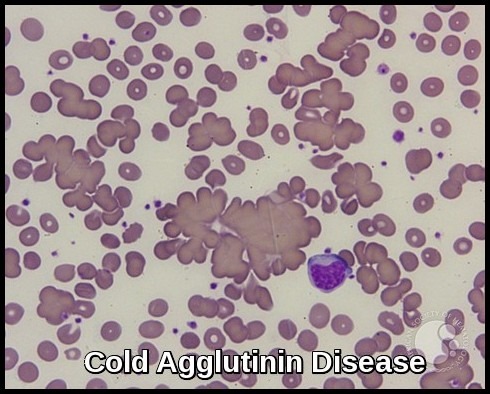
Cold Agglutinin Disease – Peripheral smear demonstrating prominent RBC agglutination due to IgM cold autoantibodies, a classic diagnostic feature of CAD.
Cold Agglutinin Disease (CAD) is a rare autoimmune hemolytic anemia (AIHA) caused by the presence of cold-reactive autoantibodies (cold agglutinins) that target red blood cells at temperatures below 30°C (86°F). These autoantibodies lead to red blood cell agglutination, complement activation, and subsequent immune-mediated hemolysis, especially in peripheral body areas exposed to cold. CAD accounts for approximately 15% of all autoimmune hemolytic anemia cases and typically affects older adults, most commonly those over 55 years of age. The disease may occur idiopathically (primary CAD) or secondary to lymphoproliferative disorders, infections, or autoimmune diseases. Early recognition of cold agglutinin syndrome, diagnostic evaluation with direct antiglobulin (Coombs) testing, and appropriate hematologic management are essential for improving outcomes and preventing cold-induced hemolytic crises.
Clinical features:
Cold agglutinin disease (CAD) manifests as acute or chronic hemolytic anemia, with associated pallor and fatigue.
Symptoms during hemolytic crises may include severe pain in the back and legs, headache, vomiting, diarrhea, dark urine, and hepatosplenomegaly.
A cold environment or a concurrent infection may trigger or exacerbate the condition, and episodes of acute hemolysis with hemoglobinemia and hemoglobinuria are more common in winter.
The disease may appear abruptly with anemia and hemoglobinuria, or onset may be more gradual and insidious.
Classification:
Cold agglutinin disease can be primary (idiopathic) or secondary, caused by an underlying condition, such as infection (Mycoplasma pneumoniae, Infectious mononucleosis, CMV), lymphoproliferative disorder, autoimmune disease or neoplasm.
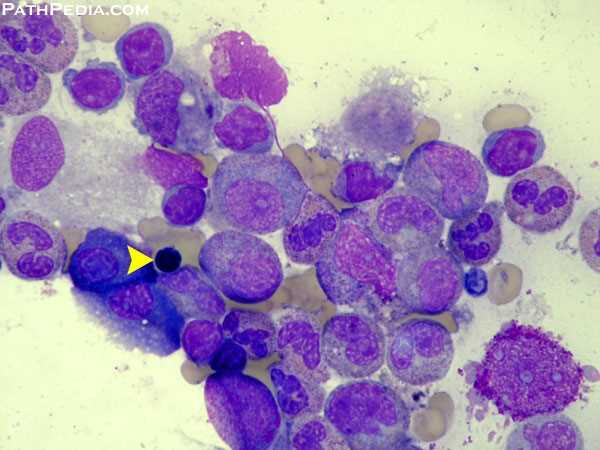
The majority of cold agglutinin disease is secondary and is due to the presence of monoclonal IgM (kappa subtype in the majority of the cases), which has the properties of a cold agglutinin and is associated with an underlying low-grade B-cell lymphoma (Waldenström’s macroglobulinemia or lymphocytic lymphoma).
Idiopathic and lymphoma-associated cold AIHA tend to be chronic while infections tend to cause an acute disease.
Diagnosis:
In some cases, the diagnosis is made by chance on a standard complete blood count (CBC) detecting abnormal agglutination of the red blood cells.
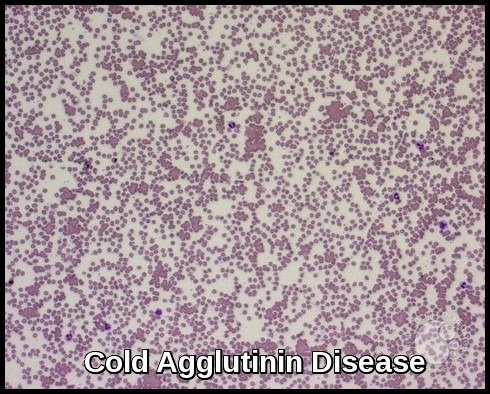
Cold Agglutinin Disease – Low-power view highlighting widespread RBC agglutination caused by IgM cold autoantibodies, a hallmark finding in CAD.
Diagnosis is based on clinical or laboratory evidence of hemolytic anemia and the detection of autoantibodies, specifically IgM, with the direct antiglobulin test (DAT, C3 positive pattern) with the presence of circulating cold agglutinins in the serum.
In contrast, warm autoimmune hemolytic anemia predominantly involves IgG.
Donath-Landsteiner hemolytic anemia is also caused by a cold-reacting immunoglobulin, but most cases are due to polyclonal IgG.
In secondary cases, lymphocytosis, with the presence of atypical lymphocytes on the smear, can be found in peripheral blood.
The differential diagnosis for cold agglutinin disease is mixed AIHA.
Investigations:
- CBC and blood film.
- Hemolysis screen: reticulocyte count, total and direct bilirubin, DAT, serum haptoglobin, serum LDH, and urine analysis for hemoglobinuria.
- Serum folate.
- Serum immunoglobulins and serum protein electrophoresis (SPEP).
- Mycoplasma, EBV, CMV, HIV, and Hepatitis C serology.
- Blood for cold agglutinins (keep the blood warm until it is tested).
- Cryoglobulin levels should be tested only if vascular purpura or other atypical findings, such as elevated levels of IgM and/or hepatitis virus antibodies, are found.
- A chest radiograph is obtained if pneumonia is suggested; pulmonary infiltrates are found in cases of Mycoplasma pneumoniae infection. Findings may also indicate lymphadenopathy. Computed tomography (CT) scans of the chest and abdomen are performed to assess for lymphadenopathy and splenomegaly when lymphoma is suggested.
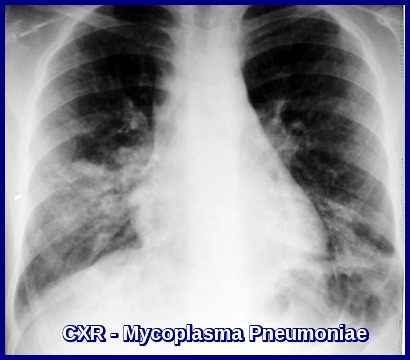
Chest X-ray in Mycoplasma pneumoniae infection demonstrating bilateral patchy interstitial infiltrates typical of atypical pneumonia, commonly associated with cold agglutinin hemolysis.
Treatment:
Patients with few clinical symptoms and mild anemia may not require treatment but only avoidance of cold. Keeping the patient warm may be sufficient treatment. Treat any underlying infection e.g. Clarithromycin or Azithromycin for Mycoplasma pneumoniae.
Anemia is generally mild. Only patients who have serious symptoms related to anemia or have a Raynaud-type syndrome that constitutes a threat to life or quality of life require active therapy.
Folic acid supplements for prevention and treatment of folate deficiency should be considered.
The disease is usually refractory to corticosteroids.
Rituximab may be an option for treatment in some cases.
In the presence of underlying lymphoma, chlorambucil or oral cyclophosphamide may be helpful.
Splenectomy is usually ineffective for the treatment of cold agglutinin disease, because the liver is the predominant site of sequestration. However, if the patient has splenomegaly, then the disease may respond to splenectomy. More importantly, a lymphoma localized to the spleen may only be found after splenectomy.
Plasmapheresis effectively, albeit temporarily, removes IgM antibody from plasma, reducing its concentration. This procedure is valuable for emergencies and allows time for drugs to have an effect. Plasmapheresis can also be used to prepare patients for hypothermic surgical procedures.
Prognosis:
The disease has a chronic course and the outcome is usually benign, except in patients with recurrent episodes of severe anemia or in whom the underlying B-cell lymphoma has an aggressive course.
Questions and Answers:
What are the key symptoms of Cold Agglutinin Disease?
Patients commonly experience fatigue, jaundice, dark urine, acrocyanosis, and worsening anemia during cold exposure due to IgM-mediated RBC agglutination.
What causes Cold Agglutinin Disease to flare in cold temperatures?
Cold exposure promotes IgM binding to red blood cells and complement activation, triggering hemolysis. Even mild cold can precipitate symptoms in moderate to severe CAD.
How is Cold Agglutinin Disease diagnosed?
Diagnosis relies on a positive DAT for C3d, elevated cold agglutinin titers, RBC agglutination on peripheral smear, raised LDH and bilirubin, and exclusion of warm AIHA or Paroxysmal Cold Hemoglobinuria.
Is Cold Agglutinin Disease linked to infections such as Mycoplasma pneumoniae?
Yes. Mycoplasma pneumoniae and Epstein–Barr virus are common secondary causes of CAD, and hemolysis usually resolves once the underlying infection is treated.
What is the recommended treatment for Cold Agglutinin Disease?
Management includes strict cold avoidance, treating infections, and in primary CAD, using therapies such as rituximab-based regimens or complement inhibitors like sutimlimab.
Can Cold Agglutinin Disease be associated with lymphoproliferative disorders?
Primary CAD frequently has an underlying clonal B-cell process, often linked to conditions such as Waldenström macroglobulinemia or low-grade lymphomas.
When is transfusion required in CAD and how is it safely administered?
Transfusion is indicated for symptomatic anemia and must be given through in-line blood warmers to prevent cold-induced agglutination during the infusion.
References:
Röth A, et al. Diagnosis and treatment of autoimmune hemolytic anemia in adults: Recommendations from the First International Consensus Meeting. Blood Reviews. 2021;47:100789. doi:10.1016/j.blre.2020.100789.
Berentsen S, et al. Current challenges and future prospects in cold-antibody hemolytic anemia. Journal of Blood Medicine. 2020;11:13–25. doi:10.2147/JBM.S189231.
Berentsen S, Randen U, Tjønnfjord GE. Cold agglutinin–mediated autoimmune hemolysis. Hematology/Oncology Clinics of North America. 2015;29(3):455–471.
Swiecicki PL, Hegerova LT, Gertz MA. Clinical review of IgM-mediated cold agglutinin hemolysis. Blood. 2013;122(7):1114–1121.
Agarwal SK, Ghosh PK, Gupta D. Cardiac surgery considerations in patients with cold-reactive proteins. Annals of Thoracic Surgery. 1995;60(4):1143–1150.
Dacie J. The autoimmune haemolytic anaemias. In: The Haemolytic Anaemias. 3rd ed. Edinburgh: Churchill Livingstone; 1992. Vol 3:210–362.
Aljubran SA, Kaliner MA. Overview of cold-antibody autoimmune hemolysis: Background, pathophysiology, and etiology. Medscape. Accessed September 2016.
https://emedicine.medscape.com/article/135327-overview
Marc Michel. Overview of cold-antibody hemolytic anemia (Orphanet Encyclopedia). Accessed January 2010.
https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=56425
American Society of Hematology (ASH). ASH Image Bank — RBC agglutination image set for CAD. Accessed January 2010.
https://imagebank.hematology.org/imageset/909/cold-agglutininin-disease
National Institutes of Health (NIH) / MedlinePlus. Patient information on cold-induced hemolytic anemia.
https://medlineplus.gov/ency/article/000578.htm
National Organization for Rare Disorders (NORD). Rare disease overview and management guidance for cold-antibody hemolysis.
https://rarediseases.org/rare-diseases/cold-agglutinin-disease
Centers for Disease Control and Prevention (CDC). Clinical overview of autoimmune hemolytic anemia.
https://www.cdc.gov/blooddisorders
Keywords:
cold agglutinin disease, CAD, cold agglutinin hemolytic anemia, cold autoimmune hemolysis, cold-antibody hemolysis, cold agglutinin–mediated anemia, cold antibody anemia, primary cold agglutinin disease, secondary cold agglutinin disease, cold agglutinin syndrome, cold-induced hemolysis, cold trigger hemolysis, cold agglutinin titers, thermal amplitude cold agglutinins, complement-mediated hemolysis, IgM cold autoantibodies, C3d DAT positive, peripheral smear red cell agglutination, cold agglutinin disease diagnosis, DAT C3 positive anemia, cold agglutinin disease symptoms, acrocyanosis cold agglutinin disease, cold agglutinin disease in adults, cold agglutinin disease complications, cold agglutinin disease management, warming blood transfusion CAD, cold agglutinin disease treatment, rituximab for CAD, sutimlimab cold agglutinin disease, Mycoplasma pneumoniae cold agglutinins, atypical pneumonia hemolysis, cold agglutinin disease prognosis, hemolytic anemia cold exposure, immune hemolytic anemia cold, hematology cold agglutinin, Ask Hematologist cold agglutinin disease, Dr Moustafa Abdou

Request Online Consultation With Dr M Abdou
Fee: US$100
Secure payment via PayPal (credit and debit cards accepted)
Pay Now