Multiple Myeloma
First described in 1848, multiple myeloma (MM), also known as plasma cell myeloma, is characterized by a proliferation of malignant plasma cells and a subsequent overproduction of monoclonal paraprotein (M protein).
There are several types of plasma cell neoplasms. These diseases are all associated with a monoclonal (or myeloma) protein (M protein). They include monoclonal gammopathy of undetermined significance (MGUS), isolated plasmacytoma of the bone, extramedullary plasmacytoma, multiple myeloma, and plasma cell leukemia. The ICD 10 code for multiple myeloma and malignant plasma cell neoplasms is C90.
The incidence of multiple myeloma is 2 to 4/100,000. Male:Female ratio is 1.6:1, and the median age is about 65 years. Prevalence in blacks is twice that in whites. Etiology is unknown, although chromosomal and genetic factors, radiation, and chemicals have been suggested.
Estimated new cases and deaths from multiple myeloma in the United States in 2016:
- New cases: 30,330.
- Deaths: 12,650.
Clinical features:
The presentation of multiple myeloma can range from asymptomatic to severely symptomatic, with complications requiring urgent treatment. Many patients are identified when routine laboratory tests show an elevated total protein level in the blood or anemia. Systemic complications include bleeding, infection, and renal failure; pathologic fractures and spinal cord compression may occur.
Presenting symptoms of MM include the following:
- Bone pain: The most common symptom of myeloma is bone pain. About 7 in 10 people (70%) have lower back or rib pain. The lumbar spine is one of the most common sites of pain.
- Pathologic fractures: Pathologic fractures are very common in Myeloma. MM causes both generalized bone loss throughout the body and areas of bone destruction “lytic lesions” on x-rays in specific areas. The bone loss and bony erosions can lead to osteoporosis and fractures. Many individuals with multiple myeloma experience fractures of the vertebrae, which can lead to a loss of height; about 30 percent of individuals experience fractures in other bones, often with little or no preceding trauma. For this reason, they are called “pathologic fractures.”
- Weakness and malaise: Anemia, which may be quite severe, is the most common cause of weakness in patients with MM.
- Bleeding and anemia: Occasionally, a patient may come to medical attention for bleeding or anemia resulting from heavy bone marrow involvement by myeloma. Rarely, monoclonal protein may absorb clotting factors and lead to bleeding.
- Infection (often pneumococcal): Abnormal humoral immunity and leucopenia may lead to infection. Pneumococcal organisms are commonly involved, but shingles (herpes zoster) and Haemophilus infections are also more common among patients with MM.
- Hypercalcemia: Because bones contain large amounts of calcium, the breakdown of bone in MM can lead to hypercalcemia. High blood calcium levels occur in 10 to 15 percent of individuals, and the symptoms may include loss of appetite, nausea, vomiting, frequent urination, increased thirst, constipation, weakness, confusion, stupor, or coma. Symptoms are more common at high calcium blood values (12.0 mg/dL or 3 mmol/l). Severe hypercalcemia (above 15–16 mg/dL or 3.75–4 mmol/l) is considered a medical emergency: at these levels, coma and cardiac arrest can result.
- Spinal cord compression: Myeloma can develop in the bones of the spine. Sometimes this can weaken the bone and put pressure on the spinal cord with spinal cord compression (SCC). SCC can cause pain, muscle weakness, and sometimes tingling and numbness of the limbs. If the lower spine is affected, it may also affect how the bowel and bladder work. The symptoms that should alert physicians to consider spinal cord compression are back pain, weakness, numbness, or dysesthesias in the extremities.
 Because spinal cord compressions in MM occur at multiple levels, comprehensive evaluation of the spine is warranted including full spine MRI scan. Patients who are ambulatory at the start of therapy have the best likelihood of preserving function and avoiding paralysis. Spinal cord compression should be treated urgently with steroids and radiotherapy. Sometimes chemotherapy can be given to help reduce the pressure on the spinal cord. Or surgery may be needed to repair or remove the affected bone.
Because spinal cord compressions in MM occur at multiple levels, comprehensive evaluation of the spine is warranted including full spine MRI scan. Patients who are ambulatory at the start of therapy have the best likelihood of preserving function and avoiding paralysis. Spinal cord compression should be treated urgently with steroids and radiotherapy. Sometimes chemotherapy can be given to help reduce the pressure on the spinal cord. Or surgery may be needed to repair or remove the affected bone.
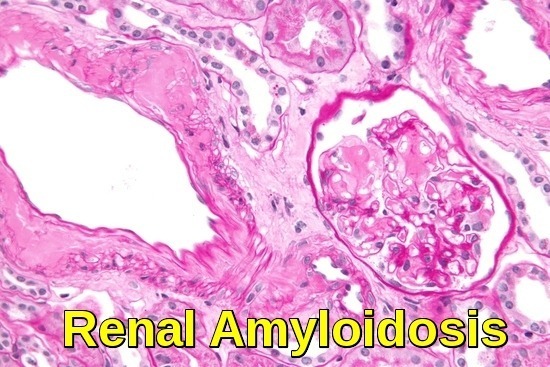
- Renal failure: In many patients, renal failure (myeloma kidney) is present at diagnosis or develops during the course of the disorder. In the majority of cases, renal impairment is caused by the accumulation and precipitation of light chains, which form casts in the distal tubules, resulting in renal obstruction. Renal failure in myeloma has many other causes e.g. hypercalcemia, recurrent renal infections, analgesic-associated nephropathy (NSAIDs), hyperuricemia, and amyloidosis. Patients also often develop anemia usually due to kidney disease or suppression of erythropoiesis by cancer cells but sometimes also due to iron deficiency.
- Hyperviscosity: Rarely, myeloma causes a very high level of paraprotein in the blood. This means the blood can become thicker than normal. Normal plasma viscosity is between 1.4 and 1.8 centipoise while symptoms from hyperviscosity typically occur greater than 4 centipoise (about 4 times more viscous than water) and require emergency treatment. Hyperviscosity may be associated with a number of symptoms, including, generalized malaise, infection, fever, paresthesia, sluggish mentation, and sensory loss. Patients may report headaches and somnolence, and they may bruise easily and have hazy vision. Patients with MM typically experience these symptoms when their serum viscosity is greater than 4 times that of normal serum. Epistaxis may be a presenting symptom of MM with a high tumor volume. Occasionally, patients may have such a high volume of monoclonal protein that their blood viscosity increases, resulting in complications such as stroke, myocardial ischemia, or infarction. Plasmapheresis may be used to decrease viscosity.
- Neurologic symptoms: Carpal tunnel syndrome is a common complication of myeloma. Meningitis (especially that resulting from pneumococcal or meningococcal infection) is more common in patients with MM. Some peripheral neuropathies have been attributed to MM. Long-term neurologic function is directly related to the rapidity of the diagnosis and the institution of appropriate therapy for multiple myeloma.
Pathophysiology:
The M-protein produced by the malignant plasma cells is IgG in about 55% of myeloma patients and IgA in about 20%; of patients producing either IgG or IgA, 40% also have Bence Jones proteinuria, which is free monoclonal kappa (κ) or lambda (λ) light chains in the urine. In 15 to 20% of patients, plasma cells secrete only Bence Jones protein (light chain myeloma). IgD myeloma accounts for about 1% of cases. Rarely, patients have no M-protein in blood and urine, although a new serum free light chain assay now demonstrates monoclonal light chains in many of these patients.
Diffuse osteoporosis or discrete osteolytic lesions develop, usually in the pelvis, spine, ribs, and skull. Lesions are caused by bone replacement by expanding plasmacytomas or by cytokines that are secreted by malignant plasma cells that activate osteoclasts and suppress osteoblasts. The osteolytic lesions are usually multiple; occasionally, they are solitary intramedullary masses. Increased bone loss may also lead to hypercalcemia. Extramedullary solitary plasmacytomas are unusual but may occur in any tissue, especially in the upper respiratory tract.
In many patients, renal failure (myeloma kidney) is present at diagnosis or develops during the course of the disorder. Renal failure has many causes, most commonly, it results from deposition of light chains in the distal tubules or hypercalcemia. Patients also often develop anemia usually due to kidney disease or suppression of erythropoiesis by cancer cells but sometimes also due to iron deficiency.
Susceptibility to bacterial infection may occur in some patients. Viral infections, especially herpes zoster infections, are increasingly occurring as a result of newer treatment modalities, especially use of the proteasome inhibitors bortezomib (Velcade) and carfilzomib (Kyprolis).
It is estimated that 10 to 15 percent of multiple myeloma patients will experience symptoms from the development of amyloidosis during the course of their disease. However, as many as 38 percent of myeloma patients may develop amyloidosis but experience none of its symptoms. Amyloidosis is a disease in which proteins accumulate in organs such as the heart, kidney, liver, nerves or intestines, leading to organ damage.
Diagnosis:
Multiple myeloma is suspected in patients >40 years with persistent unexplained bone pain, particularly at night or at rest, other typical symptoms, or unexplained laboratory abnormalities, such as elevated blood protein or urinary protein, hypercalcemia, renal insufficiency, or anemia.
Anemia is present in 80% of patients, usually normocytic-normochromic anemia with formation of rouleau, which are clusters of 3 to 12 RBCs that occur in stacks. WBC and platelet counts are usually normal. ESR usually is > 100 mm/h; BUN, serum creatinine, LDH, and serum uric acid may be elevated. Anion gap is sometimes low. Hypercalcemia is present at diagnosis in about 10% of patients.
Protein electrophoresis is done on a serum sample and on a urine sample concentrated from a 24-h collection to quantify the amount of urinary M-protein. Serum electrophoresis identifies M-protein in about 80 to 90% of patients. The remaining 10 to 20% are usually patients with only free monoclonal light chains (Bence Jones or light chain myeloma) or IgD. They almost always have M-protein detected by urine protein electrophoresis.
Immunofixation electrophoresis can identify the immunoglobulin class of the M-protein (IgG, IgA, or uncommonly IgD, IgM, or IgE) and can often detect light-chain protein if serum immunoelectrophoresis is falsely negative; immunofixation electrophoresis is done even when the serum test is negative if multiple myeloma is strongly suspected.
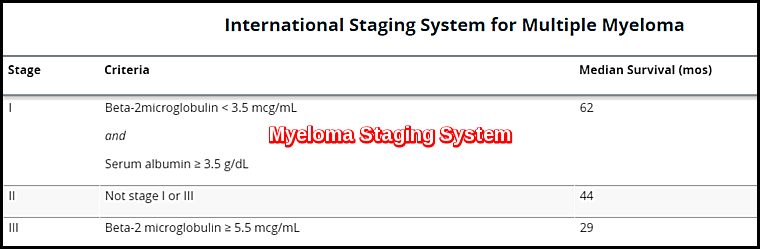
Serum free light-chain analysis with delineation of kappa and lambda ratios helps confirm the diagnosis and can also be used to monitor efficacy of therapy and provide prognostic data. Serum level of beta-2 microglobulin is measured if diagnosis is confirmed or very likely and along with serum albumin is used to stage patients as part of the international staging system for multiple myeloma.
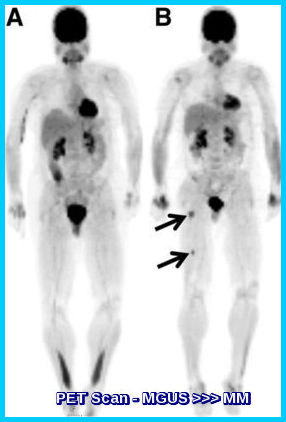
X-rays include a skeletal survey (plain x-rays of skull, long bones, spine, pelvis, and ribs). Punched-out lytic lesions or diffuse osteoporosis is present in 80% of cases. Radionuclide bone scans usually are not helpful. MRI can provide more detail and is obtained if specific sites of pain or neurologic symptoms are present. PET-CT may provide prognostic information and can help determine whether patients have solitary plasmacytoma or multiple myeloma.
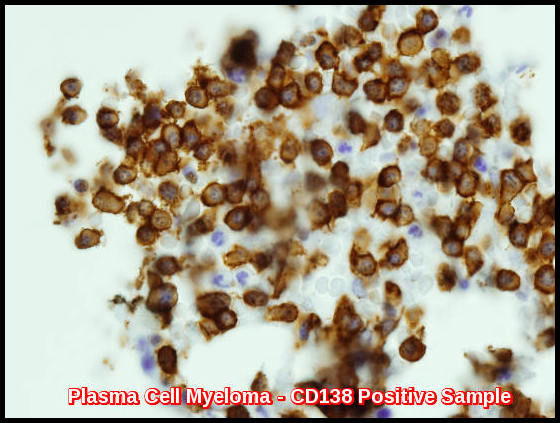
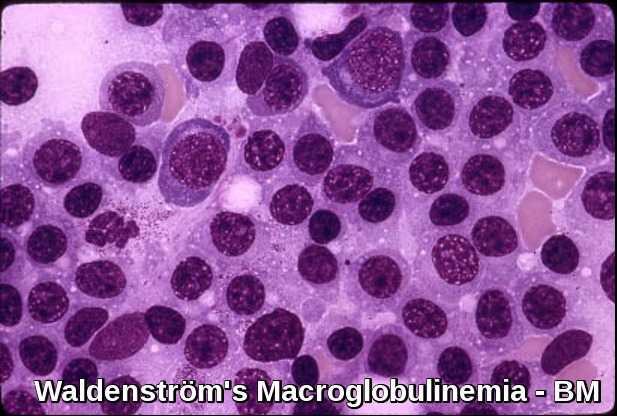
Bone marrow aspiration and biopsy are done and reveal sheets or clusters of plasma cells; myeloma is diagnosed when >10% of the cells are of this type. However, bone marrow involvement is patchy; therefore, some samples from patients with myeloma may show <10% plasma cells. Still, the number of plasma cells in bone marrow is rarely normal. Plasma cell morphology does not correlate with the class of immunoglobulin synthesized. Chromosomal studies on bone marrow (eg, using cytogenetic testing methods such as fluorescent in situ hybridization [FISH] and immunohistochemistry) may reveal specific karyotypic abnormalities in plasma cells associated with differences in survival.
Diagnosis and differentiation from other malignancies (e.g. metastatic carcinoma, lymphoma, leukemia) and monoclonal gammopathy of undetermined significance typically requires multiple criteria:
- Clonal bone marrow plasma cells or plasmacytoma
- M-protein in plasma and/or urine
- Organ impairment (hypercalcemia, renal insufficiency, anemia, or bony lesions)
In patients without serum M protein, myeloma is indicated by Bence Jones proteinuria > 300 mg/24 h or abnormal serum free light chains, osteolytic lesions (without evidence of metastatic cancer or granulomatous disease), and sheets or clusters of plasma cells in the bone marrow.
The 2014 International Myeloma Working Group guidelines for the standard investigative workup in patients with suspected multiple myeloma include the following studies:
- FBC, peripheral blood smear, ESR, and chemistry panel (BUN, creatinine, calcium, uric acid).
- Serum and urine assessment for monoclonal protein.
- Serum free light chain assay.
- Bone marrow aspiration and/or biopsy.
- Serum beta2-microglobulin, albumin, serum immunoglobulins, and lactate dehydrogenase (LDH) measurement.
- Standard metaphase cytogenetics.
- Fluorescence in situ hybridization (FISH).
- Skeletal survey.
- Magnetic resonance imaging (MRI), fluorodeoxyglucose-positron emission tomography (FDG-PET), or low-dose whole-body CT for better detection of bone and extramedullary disease.
Current National Comprehensive Cancer Network (NCCN) clinical practice guidelines on multiple myeloma also recommend the use of FISH for 1q21 amplification as part of the initial diagnostic workup.
Diagnostic criteria:
In the updated 2010 International Myeloma Working Group (IMWG) diagnostic criteria, plasma cell MGUS is defined as having serum M-protein < 30 g/L, clonal plasma cell population in bone marrow < 10%, and absence of end-organ damage (CRAB criteria of multiple myeloma).
Multiple myeloma is defined as smoldering (asymptomatic) or active (symptomatic).
Criteria for smoldering multiple myeloma are as follows:
- M-protein in serum: IgG ≥30 g/L, IgA >10 g/L or
- Bence-Jones protein >1 g/24h and/or
- Bone marrow clonal plasma cells ≥10%
- Calcium >11.5 mg/dL (>2.65 mmol/L)
- Creatinine >2 mg/dL (177 μmol/L or more)
- Hemoglobin <10 g/dL or 2 g/dL <normal
- Lytic or osteopenic bone disease
In November 2014, however, the International Myeloma Working Group added the following criteria for multiple myeloma that will require therapy:
- Bone marrow plasma cells (BMPCs) ≥60%
- Involved/uninvolved serum free light chain ratio ≥100
- Abnormal MRI with more than one focal lesion, with each lesion >5 mm
The International Working Group noted that these findings have been “associated with near inevitable development of CRAB features in patients who would otherwise be regarded as having smouldering multiple myeloma.” The presence of any of the CRAB criteria or any of these three additional criteria justifies therapy.
Treatment:
Solitary plasmacytomas:
These are often treated with radiation therapy. If the plasma cell tumor is not in a bone, it may be removed with surgery. Chemotherapy is only used if multiple myeloma develops.
Early myeloma:
Early myeloma includes smoldering myeloma and stage I disease. Patients with early myeloma can do well for years without treatment. For many patients, starting treatment early does not seem to help them live longer. These patients are often watched closely (Watchful Waiting) without starting chemotherapy or other treatments for myeloma. They may be started on a bisphosphonate (e.g. Zoledronic Acid or Pamidronate monthly infusions) if they have bone disease.
Based on how abnormal the plasma cells look under the microscope and the levels of immunoglobulins, some patients with early myeloma have a high risk of progressing to active myeloma and needing treatment. In one study, treating these patients with lenalidomide (Revlimid) and dexamethasone before they developed symptoms or problems helped them live longer.
Active (symptomatic) myeloma:
Patients whose myeloma is stage II or higher or who have light chain amyloidosis are often given drug therapy. The drugs chosen depend on the patient’s health (including their kidney function) and whether a transplant is planned.
Often, a combination containing bortezomib (Velcade), thalidomide or lenalidomide, and dexamethasone is used. Combinations containing bortezomib are especially helpful in patients with kidney problems and those whose myeloma cells contain certain high risk chromosome abnormalities.
If the patient is not expected to have a transplant, chemotherapy with melphalan and prednisone (MP) may be used, and can be combined with thalidomide (MPT) or with velcade (MPV).
Many drug combinations can be useful in treating myeloma. If a drug stops working (or the myeloma comes back), others can be tried.
Bisphosphonate treatment is often started along with chemotherapy. If the areas of damaged bone continue to cause symptoms, radiation therapy may be used.
Patients with multiple myeloma also receive supportive treatments, such as transfusions to treat low blood cell counts, and antibiotics and sometimes intravenous immunoglobulin (IVIG) for infections.
Immunomodulating agents:
The way immunomodulating agents affect the immune system isn’t entirely clear. Three immunomodulating agents are used to treat multiple myeloma. The first of these drugs to be developed, thalidomide, caused severe birth defects when taken during pregnancy. Because the other immunomodulating agents are related to thalidomide, there’s concern that they could also cause birth defects. That’s why all of these drugs can only be obtained through a special program run by the drug company that makes them.
Because these drugs can increase the risk of serious blood clots, they are often given along with aspirin or a blood thinner.
Thalidomide (Thalomid) was first used decades ago as a sedative and as a treatment for morning sickness in pregnant women. When it was found to cause birth defects, it was taken off the market. Later, it became available again as a treatment for multiple myeloma. Side effects of thalidomide can include drowsiness, fatigue, severe constipation, and painful nerve damage (neuropathy). The neuropathy can be severe, and might not go away after the drug is stopped. There is also an increased risk of serious blood clots that start in the leg and can travel to the lungs.
Lenalidomide (Revlimid) is a similar to thalidomide. It works well in treating multiple myeloma. The most common side effects of lenalidomide are thrombocytopenia and leucopenia. It can also cause painful nerve damage. The risk of blood clots is not as high as that seen with thalidomide, but it is still increased.
Pomalidomide (Pomalyst) is related to thalidomide and is used to treat multiple myeloma. Some common side effects include anemia and leucopenia. The risk of nerve damage (neuropathy) is not as severe as it is with the other immunomodulating drugs, but it’s also linked to an increased risk of blood clots.
Proteasome inhibitors:
Proteasome inhibitors work by stopping enzyme complexes (proteasomes) in cells from breaking down proteins important for keeping cell division under control. They appear to affect tumor cells more than normal cells, but they are not without side effects.
Bortezomib (Velcade) was the first of this type of drug to be approved, and it’s often used to treat multiple myeloma. It may be especially helpful in treating myeloma patients with kidney problems. It’s injected into a vein (IV) or under the skin, once or twice a week. Common side effects of this drug include nausea and vomiting, tiredness, diarrhea, constipation, fever, decreased appetite, and lowered blood counts. The platelet count (which can cause easier bruising and bleeding) and the white blood cell count (which can increase the risk of serious infection) are most often affected. Bortezomib can also cause nerve damage (peripheral neuropathy) that can lead to problems with numbness, tingling, or even pain in the hands and feet. Some patients develop shingles (herpes zoster) while taking this drug. To help prevent this, an anti-viral medicine (like acyclovir) may be prescribed.
Carfilzomib (Kyprolis) is a newer proteasome inhibitor that can be used to treat multiple myeloma in patients who have already been treated with bortezomib and an immunomodulating agent. It’s given as an injection into a vein (IV), often in a 4 week cycle. To prevent problems like allergic reactions during the infusion, the steroid drug dexamethasone is often given before each dose in the first cycle. Common side effects include tiredness, nausea and vomiting, diarrhea, shortness of breath, fever, and low blood counts. People on this drug can also have more serious problems, such as pneumonia, heart problems, and kidney or liver failure.
Ixazomib (Ninlaro) is a proteasome inhibitor that is taken by mouth as a capsule, typically once a week for 3 weeks, followed by a week off. This drug is usually used after other drugs have been tried. Common side effects of this drug include nausea and vomiting, diarrhea, constipation, rash, swelling in the hands or feet, back pain, and a lowered blood platelet count. This drug can also cause nerve damage (peripheral neuropathy) that can lead to problems with numbness, tingling, or even pain in the hands and feet.
Histone deacetylase (HDAC) inhibitors: are a group of drugs that can affect which genes are active inside cells. They do this by interacting with proteins in chromosomes called histones. Panobinostat (Farydak) is an HDAC inhibitor that can be used to treat patients who have already been treated with bortezomib and an immunomodulating agent. It is taken as a capsule, typically 3 times a week for 2 weeks, followed by a week off. This cycle is then repeated. Common side effects include diarrhea (which can be severe), feeling tired, nausea, vomiting, loss of appetite, swelling in the arms or legs, fever, and weakness. This drug can also affect blood cell counts and the levels of certain minerals in the blood. Less common but more serious side effects can include bleeding inside the body, liver damage, and changes in heart rhythm, which can sometimes be life threatening.
Monoclonal Antibodies:
Daratumumab (Darzalex) is a monoclonal antibody that attaches to the CD38 protein, which is found on myeloma cells. This is thought to both kill the cells directly and to help the immune system attack the cells. This drug is used mainly in patients who have already had several other treatments for their myeloma. It’s given as an infusion into a vein. This drug can cause a reaction in some people while it is being given or within a few hours afterward, which can sometimes be severe. Symptoms can include coughing, wheezing, trouble breathing, tightness in the throat, a runny or stuffy nose, feeling dizzy or lightheaded, headache, rash, and nausea. Other side effects can include fatigue, nausea, back pain, fever, and cough. This drug can also lower blood cell counts, which can increase the risk of infections and bleeding or bruising.
Darzalex (daratumumab) in combination with bortezomib, thalidomide, and dexamethasone (VTD) has been granted approval for the treatment of patients with newly diagnosed multiple myeloma who are eligible for autologous stem cell transplant (ASCT).
Elotuzumab (Empliciti) is a monoclonal antibody that attaches to the SLAMF7 protein, which is found on myeloma cells. This is thought to help the immune system attack the cells. This drug is used mainly in patients who have already had other treatments for their myeloma. It’s given as an infusion into a vein. This drug can cause a reaction in some people while it is being given or within several hours afterward, which can sometimes be severe. Symptoms can include fever, chills, feeling dizzy or lightheaded, rash, wheezing, trouble breathing, tightness in the throat, or a runny or stuffy nose. Other common side effects with this drug include fatigue, fever, loss of appetite, diarrhea, constipation, cough, nerve damage resulting in weakness or numbness in the hands and feet (peripheral neuropathy), upper respiratory tract infections (such as a cold), and pneumonia.
Stem Cell Transplant for Multiple Myeloma:
In a stem cell transplant, the patient gets high-dose chemotherapy (sometimes with radiation to the whole body) to kill the cells in the bone marrow (including the myeloma cells). Then the patient receives new, healthy blood-forming stem cells. When stem cell transplants were first developed, the new stem cells came from bone marrow, and so this was known as a bone marrow transplant. Now, stem cells are more often gathered from the blood (a peripheral blood stem cell transplant).
Stem cell transplant is commonly used to treat multiple myeloma. Before the transplant, drug treatment is used to reduce the number of myeloma cells in the patient’s body.
Stem cell transplants (SCT) are autologous and allogeneic.
Autologous transplants
For an autologous stem cell transplant, the patient’s own stem cells are removed from his or her bone marrow or peripheral blood before the transplant. The cells are stored until they are needed for the transplant. Then, the person with myeloma gets treatment such as high-dose chemotherapy e.g. Melphalan, sometimes with radiation, to kill the cancer cells. When this is complete, the stored stem cells are infused back into the patient’s blood.
This type of transplant is a standard treatment for patients with multiple myeloma. Still, while an autologous transplant can make the myeloma go away for a time (even years), it doesn’t cure the cancer, and eventually the myeloma returns.
Some doctors recommend that patients with multiple myeloma have 2 autologous transplants, 6 to 12 months apart. This approach is called tandem transplant. Studies show that this may help some patients more than a single transplant. The drawback is that it causes more side effects and so is riskier.
Allogeneic transplants
In an allogeneic stem cell transplant, the patient gets blood-forming stem cells from another person – the donor. The best treatment results occur when the donor’s cells are closely matched to the patient’s cell type and the donor is closely related to the patient, such as a brother or sister. Allogeneic transplants are much riskier than autologous transplants, but they may be better at fighting the cancer. That’s because transplanted (donor) cells may actually help destroy myeloma cells. This is called a graft vs. tumor effect. Still, in studies of multiple myeloma patients, those who got allogeneic transplants often did worse in the short term than those who got autologous transplants. At this time, allogeneic transplants are not considered a standard treatment for myeloma, but may be done as a part of a clinical trial.
The early side effects from a stem cell transplant (SCT) are similar to those from chemotherapy and radiation, only more severe. One of the most serious side effects is low blood counts, which can lead to risks of serious infections and bleeding.
The most serious side effect from allogeneic transplants is graft-versus-host disease (or GVHD). This occurs when the new immune cells (from the donor) see the patient’s tissues as foreign and so attack them. GVHD can affect any part of the body and can be life threatening.
Some patients are given additional cycles of treatment after transplant. This is called consolidation treatment and increases the chance of a complete response (where signs and symptoms of the disease go away).
Some patients (even some who didn’t have a stem cell transplant) may be given long-term treatment with thalidomide, lenalidomide, or bortezomib. This is known as maintenance treatment, and helps delay the return of the myeloma, but it can cause serious side effects.
CAR T-Cell Therapy for Multiple Myeloma:
CAR T-cell therapy is a promising treatment for patients with multiple myeloma, whose disease has relapsed or is not responding to (refractory) prior treatments. It is a highly-specialized therapy that involves genetically modifying a patient’s own T cells to attack their multiple myeloma using a target called B-cell maturation antigen (BCMA). The FDA has approved CAR T-cell therapy for multiple myeloma. Dana-Farber Brigham Cancer Center is a leader in bringing new CAR T-cell therapies to patients in need and led the clinical trial that led to FDA approval of CAR T for multiple myeloma.
CAR T-cell therapy is approved for multiple myeloma that has relapsed after or is refractory to at least four prior treatments. The clinical trial showed the CAR T-cell therapy to be highly effective for patients whose disease had relapsed after or not responded to multiple prior treatments.
Prognosis:
The disease is progressive and incurable, but median survival has recently improved to > 5 years as a result of advances in treatment. Unfavorable prognostic signs at diagnosis are lower serum albumin and higher beta-2 microglobulin levels. Patients initially presenting with renal failure also do poorly unless kidney function improves with therapy (which typically happens with current treatment options). Certain cytogenetic abnormalities increase risk of poor outcome.
Because multiple myeloma is ultimately fatal, patients are likely to benefit from discussions of end-of-life care that involve their doctors and appropriate family and friends. Points for discussion may include advance directives, the use of feeding tubes, and pain relief.
A new, real-world study of around 11,000 multiple myeloma patients across three Nordic countries finds that autologous stem cell transplantation (ASCT) was associated with the longest survival of nearly 8-10 years.
Travel Insurance:
Dhaval Shah, MD Multiple Myeloma: Practice Essentials, Background, Pathophysiology http://emedicine.medscape.com/article/204369-overview. Last accessed December 8, 2016.
James R. Berenson, MD Multiple Myeloma – Hematology and Oncology – Merck Manuals Professional Edition http://www.merckmanuals.com/professional/hematology-and-oncology/plasma-cell-disorders/multiple-myeloma. Last accessed September, 2016.
Bekelman, J; Jackson, N; Donehower, R (2006). Oncologic emergencies (2nd ed.). Philadelphia: Saunders Elsevier.
Rajkumar SV, Kumar S. Multiple myeloma: diagnosis and treatment. Mayo Clinic Proc91(1):101-119, 2016.doi: 10.1016/j.mayocp.2015.11.007.
Melissa Cobleigh PhD (2010): Multiple Myeloma-Associated Amyloidosis – What Every Patient Should Know www.myelomabeacon.com/news/2010/09/15/multiple-myeloma-associated-amyloidosis-what-every-patient-should-know/
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology Multiple Myeloma. V4.2015. NCCN. Available at http://www.nccn.org/professionals/physician_gls/pdf/myeloma.pdf. Accessed: June 23, 2015.
American Cancer Society: Treatment Options for Multiple Myeloma, by Stage https://www.cancer.org/cancer/multiple-myeloma/treating/by-stage.html. Last Revised: January 19, 2016.
American Cancer Society: Cancer Facts and Figures 2016. Atlanta, Ga: American Cancer Society, 2016. Last accessed December 8, 2016.
CAR T-Cell Therapy for Multiple Myeloma – Dana-Farber Cancer Institute | Boston, MA https://www.dana-farber.org/cellular-therapies-program/car-t-cell-therapy/car-t-cell-therapy-for-multiple-myeloma/
Miriam Davis. Multiple Myeloma: What Treatments Work Best in the Real World? – Medscape – February 26, 2024. https://www.medscape.com/s/viewarticle/multiple-myeloma-what-treatments-work-best-real-world-2024a10003kg?src=rss
Keywords:
Myeloma symptoms, Myeloma treatment options, Plasma cell myeloma, Myeloma diagnosis, Myeloma prognosis, Myeloma risk factors, Immunoglobulin myeloma, Monoclonal gammopathy, Myeloma research advancements, Myeloma awareness, Myeloma support, multiple myeloma cancer, myeloma definition, myeloma what is it, myeloma treatment, myeloma news, myeloma blood cancer, myeloma medical definition, myeloma icd 10, myeloma cancer treatment, myeloma cancer survival rate, myeloma cancer causes, myeloma cancer stages, myeloma cancer blood test, multiple myeloma definition simple, smoldering myeloma what is it, smouldering myeloma what is it, is myeloma terminal, is myeloma dangerous, how is myeloma detected, myeloma travel insurance, multiple myeloma travel insurance, mgus and travel insurance, can you get travel insurance if you have myeloma, can you get travel insurance if you have cancer, can you travel with multiple myeloma.











Hello,
I’m looking for some advice if you’re able to give me any. I have sharp pain in my hips when I walk and very tired. I just got a pelvic x Ray. The report came normal but I see a small possible lesion. If it is something I’m trying to catch it early. My calcium is at 10.1 right on the normal high mark. My anion gap has been low 2 times in the past and remains at the lowest normal mark. I see maybe 2 spots on my pelvic x Ray that could be questionable. I could send you a picture if you’re able to tell me if I should monitor it or request some lab tests. I would appreciate your help.
Hello,
Thank you for your message.
As long as the pelvic x-ray report is reassuring you don’t need to do further radiology like a skeletal survey for the time being.
However, in view of your hip pain and tiredness, I would recommend doing a CBC, ESR, U&Es, LFTs, serum immunoglobulins and serum protein electrophoresis to be sure that everything is okay.
Regards,
My husband (65) has recent progression to MM. MGUS in 2014. blood work was normal in December 2019. January 2020 increase in M-Spike 3.5, Abnormal myelome on FISH panel monosomy on chromosome 13 gain of the 1Q21. Atypical monotypic plasma cell population (53%) consistent with neoplastic process. A CD138 (MI15) stain highlights 90% of cells. Positive with Lambda (SHL53) and negative Kappa (CH15) Atypical plasma cells of 63% of total cellularity. New lucent focus on anterior skill of 2 cm. 90% involvement. VRD failed. Added Ninlaro, failed. Now on DKD for 4 weeks.
Recent labs show 03/30/2020
Serum Kappa
<0.7 Low
Serum Lambda
167.7 High
Kappa/Lambda Ratio,S
<.00 Low
IgG
174 Low
IgA
3269 High
IgM
8 Low
Alpha-1-Globulin
0.2
Alpha-2-Globulin
0.7
Beta Globulin
3.6 High
Gamma Globulin
0.2 Low
MSpike
2.5 High
I know that 1Q21 has a poor prognosis. But what does that really mean? I also believe I read that autologous transplant is not effective for 1Q21. We've asked about a prognosis and stage but can't seem to get any solid answers. Can you help us? More about planing than anything else.
Thank you very much for all your help.
Hi Roberta,
Thank you for your comment.
To give you a precise answer regarding staging and prognosis I need some additional information including his serum albumin, LDH, and whether or not he had a recent PET CT Scan?
Thanks,
Hello I truly believe my angels brought me to your page. I know that nobody can precisely tell me when I will my father but you can give me an idea of what to expect down the road here are his numbers from today.
Papa was diagnosed with Multiple Myeloma in Dec 2016 and was given a 6 month expectancy.
Sodium: 133
Potassium: 5.1
Chloride: 100
CO2: 28
Anion Gap: 5.0
Glucose: 103
BUN: 19
Creat: 1.2
BUN Creat Ratio: 16
Osmolality, Calculated: 269
Calcium: 8.7
Total Protein: 10.6
Albumin: 3.2
Globulin: 7.4
A/G: 0.4
Alk Phos: 79
ALT: 18
AST: 24
Total Bili: 0.3
GFR: 61
WBC: 7.1
RBC: 3.00
Hgb: 10.3
HCT: 30.5
MCV: 101.8
MCH: 34.2
MCHC: 33.6
RDW: 13.9
Plat: 123
MPV: 9.60
Gran: 67.9
Gran#: 4.8
Lymph%: 23.8
Lymph#: 1.8
MONO%: 6.
MONO#: 0.5
It would mean the world to me right now if you can give me feedback.
Hi Eve,
The information you provided here is not enough and in general, they are not bad!
The important piece of information regarding your father’s myeloma is missing!
What is the type and quantitation of the paraprotein?
How high his serum B2 microglobulin?
How is the result of his serum-free light chains?
Is there BJP in the urine?
How is the result of his PET CT scan?
BW,
Hi, I have just been diagnosed with MGUS with 2g/L monoclonal M spike …
I am on wait and see. I have rib aching, but other lab tests are in a normal range.
Can a person eat to reverse this ( I am allergic to turmeric, fish, eggs and pork)?
Hi Marg,
Thank you for your comment.
With this tiny paraprotein, you don’t need to do anything but just annual monitoring.
BW,
Thanks that is reassuring. SMILE!
Hello Dr, thank God, there’s professionals willing to help. I will appreciate very much your opinion in my situation.
On dec/19 I woke up with a vague pain in the middle of my back, in the vertebrae. Since then I have been in pain in my bones in general but also in specific parts in the skull, back, ribs, ankles; some parts of the bone in the shoulders seem to be hurt already.
I have been to different doctors but there is no sign of an end to this pain. I have been taking painkillers for the past two months.
CBC normal
Calcium normal
Urea normal
No formation roleaux
Protein normal range
Electroferesis= hypergammaglobulinemia
Total Protein normal range
Inmuno-electroferesis igg-iga-igm-kappa-lambda = no abnormalities seen
The following concerns me:
Free light chains
Kappa 403 mg/dl. H 170-370normal range
Lambda 214 mg/dL H 90-120 normal range
Ratio=1.88 ??? Out of range?????
Simple urine test=no protein
I have done imaging of what I have pain the most or most concern
Simple tórax X-ray no findings
Ct simple of tórax because of painful parts of the ribs= no litic lesions or related
Ct of skull because of pain and pins around it= normal
MRI done in may/2020 discal hernia in L5-s1
No MRI’s this year
I feel very concerned.
What should I do next?
MRI’s?
Repeat tests?
Pain has gotten worse, neuropathy too,
Fatigue and don’t feel like before at all
All tests were done 2 months ago
Hi Diego,
Thanks for your comment.
I think you did already all the investigations required to out rule myeloma.
However, I would suggest for completion of investigations to check your urine for BJP, the ESR, B2 microglobulin, LDH, along with the rheumatoid factor and ANA.
BW,