Waldenström’s Macroglobulinemia
Waldenström’s macroglobulinemia (WM), also known as Lymphoplasmacytic Lymphoma is an indolent B-cell malignancy in which there is a proliferation of small lymphocytes with some plasmacytoid differentiation. This rare form of blood cancer is characterized by an excess of abnormal white blood cells called lymphoplasmacytic cells in the bone marrow and overproduction of a protein called IgM. Waldenström’s macroglobulinemia is clinically more similar to a lymphomatous disease than to myeloma and other plasma cell disorders.
Waldenström macroglobulinemia is one of the malignant Monoclonal Gammopathies.
There is usually massive production of monoclonal IgM.
The cause of Waldenström’s macroglobulinemia is unknown. Men are affected more often than women.
Clinical features:
Waldenström’s macroglobulinemia is a disease of the elderly (median age is 65 years). After myeloma, WM is the 2nd most common malignant disorder associated with a Monoclonal Gammopathy.
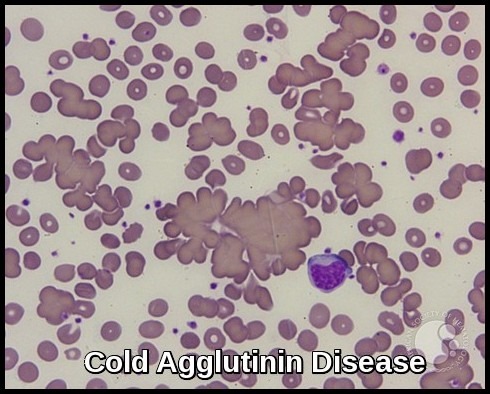
The disease usually presents with symptoms of Hyperviscosity. Symptoms of hyperviscosity include fatigue, weakness, spontaneous bleeding from mucous membranes, visual disturbances due to retinopathy, and neurologic symptoms ranging from headaches and vertigo to seizures and coma. Normal plasma viscosity is between 1.4 and 1.8 centipoise while symptoms from hyperviscosity typically occur when plasma viscosity is greater than 4 centipoise (about 4 times more viscous than water) and require emergency treatment.
weight loss is also common.
There may be hepatosplenomegaly or lymphadenopathy (cf. myeloma).
Bony lesions are not usually seen in Waldenström’s macroglobulinemia (cf. myeloma).
Investigations:
- Anemia and a high ESR are usual.
- The leucocyte count and platelet count are often normal, though malignant lymphoid cells may be seen.
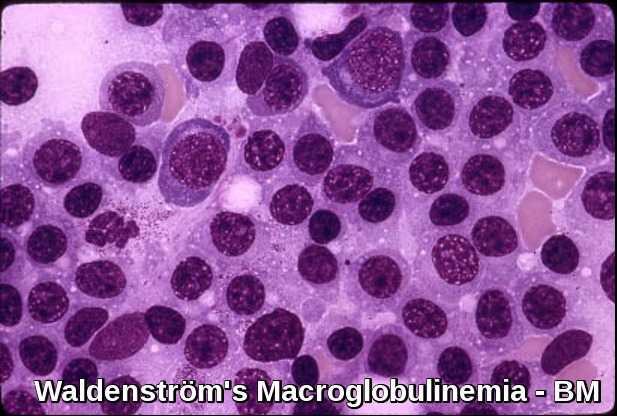
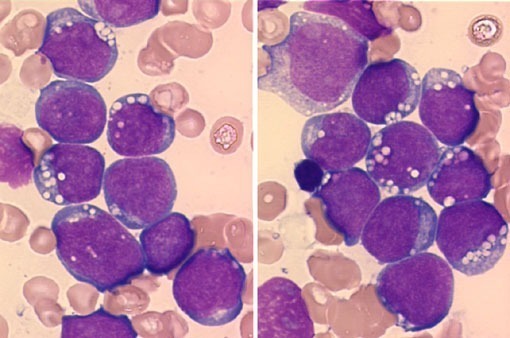
- The bone marrow shows diffuse infiltration by plasmacytoid lymphocytes. Flow cytometry results show B-cell features with surface expression of IgM and B-cell differentiation markers. In practice, a sIgM+ CD5– CD10– CD19+ CD20+ CD23–immunophenotype in association with a nonparatrabecular pattern of bone marrow infiltration is diagnostic of Waldenström’s macroglobulinemia.
- The serum IgM is usually very high and other immunoglobulins may be low.
- Cryoglobulins and Bence-Jones proteins may be present.
- Plasma viscosity is usually very high.
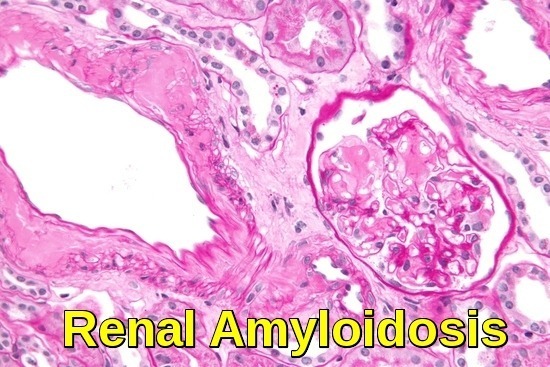
- Renal impairment is unusual (cf. myeloma).
A particular mutation in the MYD88 gene is found in more than 90 percent of people with Waldenström macroglobulinemia. The mutation involved in this condition changes a single protein building block (amino acid) in the MyD88 protein, replacing the amino acid leucine with the amino acid proline at position 265 (written as Leu265Pro or L265P). The mutation is acquired during a person’s lifetime and is present only in the abnormal white blood cells. This type of genetic change, called a somatic mutation, is not inherited. Waldenström macroglobulinemia is thought to result from multiple genetic changes, including the MYD88 gene mutation.
The altered MyD88 protein is constantly functioning (overactive). It stimulates the signaling molecules that activate nuclear factor-kappa-B, even without signals from outside the cell. Researchers suggest that abnormally active nuclear factor-kappa-B allows survival of abnormal cells that should undergo apoptosis, which may contribute to the accumulation of lymphoplasmacytic cells in Waldenström macroglobulinemia.
Treatment:
Indications for initiating active treatment for Waldenström’s macroglobulinemia include clinical evidence of adverse effects of the paraprotein (hyperviscosity with neurologic or ocular disturbance, peripheral neuropathy, amyloidosis, symptomatic cryoglobulinemia, cytopenias), disease progression (including progressive anemia), or development of constitutional symptoms.
No treatment is indicated for asymptomatic disease.
Treatment with oral alkylating drugs e.g. Chlorambucil may be indicated for palliation, but bone marrow toxicity can occur.
Corticosteroids may be effective in reducing tumor load.
Rituximab can reduce tumor burden without suppressing normal hematopoiesis. However, during the first several months, IgM levels may increase, requiring plasma exchange.
Combinations of Rituximab with Cyclophosphamide/Dexamethasone, Bendamustine, or Bortezomib/Dexamethasone provide durable responses and are indicated when treatment is required.
Nucleoside analogs (Fludarabine and 2-chlorodeoxyadenosine) produce responses in large numbers of newly diagnosed patients but have been associated with a high risk of myelodysplasia and myeloid leukemia.
New monoclonal antibodies (ofatumumab), second-generation proteasome inhibitors (carfilzomib), immunomodulatory agents (thalidomide, pomalidomide, or lenalidomide), and Bruton’s tyrosine kinase inhibitors (Ibrutinib) are promising and may expand future treatment options.
Bruton’s tyrosine kinase (BTK) plays a key role in signaling pathways for the survival of WM clone. BTK inhibition has changed the treatment landscape of the disease. Ibrutinib has resulted in deep and durable responses both as an upfront and salvage treatment with a manageable toxicity profile. However, the need for fewer off-target effects and deeper responses has resulted in the clinical development of second-generation BTK inhibitors. Zanubrutinib has resulted in clinically meaningful antitumor activity, including deep and durable responses, with a low discontinuation rate due to treatment-related toxicities. Cardiovascular adverse events seem to be milder compared with ibrutinib. Interestingly, the efficacy of zanubrutinib in WM is significant both for MYD88L265P and MYD88WT patients.

Plasmapheresis may be useful for hyperviscosity.
Autologous stem cell transplantation may be considered in young patients with chemosensitive disease and in newly diagnosed patients with very high-risk features.
Prognosis:
The course is variable, with a median survival of 7 to 10 years. Age > 60 years, anemia, and cryoglobulinemia predict shorter survival.
References:
Oza A, Rajkumar SV. Waldenstrom macroglobulinemia: prognosis and management. Blood Cancer J 5(3):e296, 2015. doi: 10.1038/bcj.2015.28.
James R. Berenson, MD Macroglobulinemia – Hematology and Oncology – Merck Manuals Professional Edition http://www.merckmanuals.com/professional/hematology-and-oncology/plasma-cell-disorders/macroglobulinemia Accessed: September 2016.
Vogt RF, Marti GE. Overview of monoclonal gammopathies of undetermined significance. Br J Haematol. 2007 Dec. 139(5):687-9.
MYD88 gene: MedlinePlus Genetics https://medlineplus.gov/genetics/gene/myd88/
Ntanasis-Stathopoulos I, Gavriatopoulou M, Fotiou D, Dimopoulos MA. Current and novel BTK inhibitors in Waldenström’s macroglobulinemia. Ther Adv Hematol. 2021 Feb 7;12:2040620721989586. doi: 10.1177/2040620721989586. PMID: 33613931; PMCID: PMC7874350.