Acanthocytosis
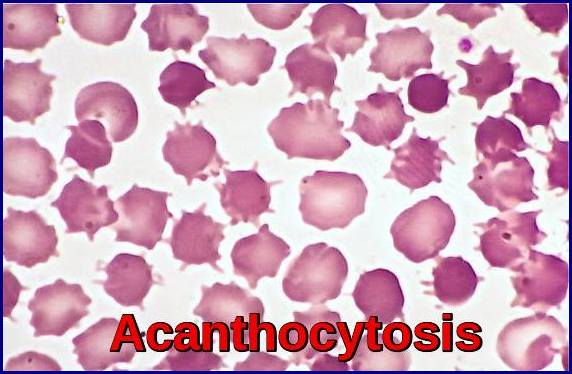
Acanthocytosis demonstrated by multiple spur cells (acanthocytes) with irregular membrane projections on a peripheral blood smear.
Acanthocytes, also known as spur cells, are abnormal red blood cells characterized by irregularly spaced, variably sized membrane projections, reflecting a true structural alteration of the erythrocyte membrane rather than a reversible shape change. The development of acanthocytosis results from disruption of the lipid composition and reduced fluidity of the red cell membrane, most commonly due to an increased cholesterol-to-phospholipid ratio. Acanthocytosis may occur as an inherited autosomal recessive disorder or as an acquired condition, and is classically associated with abetalipoproteinemia, neuroacanthocytosis syndromes, advanced liver disease, and severe malnutrition. In abetalipoproteinemia, a rare autosomal recessive lipid transport disorder, defective absorption of fat-soluble vitamins—particularly vitamin E—leads to a progressive spinocerebellar neurodegenerative syndrome with peripheral neuropathy and retinitis pigmentosa, alongside the characteristic appearance of acanthocytes on the peripheral blood film.

Retinitis pigmentosa with characteristic bone spicule pigmentation seen in inherited acanthocytosis and abetalipoproteinemia.
Chorea-acanthocytosis is a rare hereditary neurodegenerative disorder characterized by progressive movement abnormalities and the presence of acanthocytes on the peripheral blood smear. The term chorea refers to the involuntary, irregular, jerky movements that affect multiple body regions, commonly involving the face, limbs, and trunk. This condition belongs to the broader group of disorders known as neuroacanthocytosis syndromes, which combine severe neurological dysfunction with abnormal spiculated red blood cells.
In addition to inherited neuroacanthocytosis, acanthocytes may also be observed in several acquired systemic conditions, most notably advanced liver cirrhosis, chronic renal failure, microangiopathic hemolytic anemia, and occasionally as a laboratory artifact in blood samples stored in EDTA, where echinocytic changes may mimic true acanthocytosis.
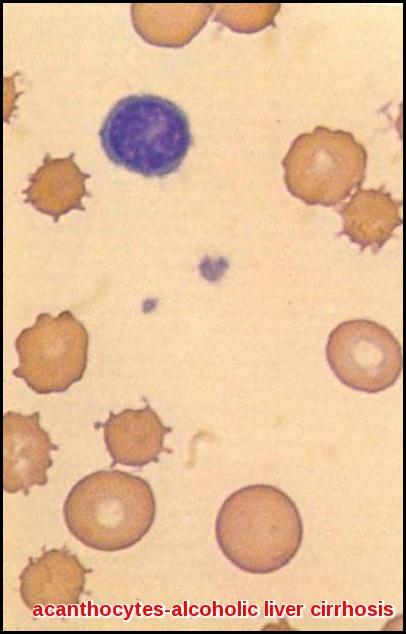
Acanthocytosis with multiple spur cells (acanthocytes) seen on peripheral blood smear in alcoholic liver cirrhosis.
Acanthocytes must be carefully distinguished from echinocytes (burr cells), as the two red cell abnormalities differ fundamentally in morphology, pathophysiology, and clinical significance. Echinocytes, commonly known as burr cells, are characterized by numerous short, evenly spaced, uniform surface projections distributed symmetrically around the red blood cell membrane, in contrast to the irregular, variably sized projections of acanthocytes. Importantly, echinocytic transformation is typically reversible, reflecting extrinsic environmental influences rather than a fixed membrane defect; these changes may result from alterations in plasma pH, osmolarity, metabolic stress, the surface properties of glass slides used for smear preparation, or exposure to certain chemical agents and anticoagulants.

Echinocytes (burr cells) with multiple short, evenly distributed surface projections on a peripheral blood smear.
Echinocytes (burr cells) are encountered in a wide range of clinical and metabolic conditions, most commonly in malnutrition-associated states complicated by mild hemolysis secondary to hypomagnesemia and hypophosphatemia, as well as in uremia, exercise-induced hemolytic anemia in long-distance runners, and inherited red cell enzyme disorders such as pyruvate kinase deficiency. In addition to these in vivo associations, echinocytosis frequently develops in vitro as an artifact related to elevated blood pH, prolonged blood storage, ATP depletion, intracellular calcium accumulation, and mechanical interaction with glass surfaces during smear preparation, all of which promote reversible membrane surface changes rather than true structural lipid abnormalities.
Summary:
Acanthocytosis is a red blood cell abnormality in which the cells develop irregular, spiky projections known as acanthocytes or spur cells. This post explains what acanthocytosis looks like on the blood smear, how it differs from echinocytes (burr cells), and why it happens due to changes in the red cell membrane. It covers the most important causes, including inherited conditions such as abetalipoproteinemia and neuroacanthocytosis, as well as acquired disorders such as advanced liver cirrhosis, kidney failure, and hemolytic anemia. The article also discusses the neurological features of chorea-acanthocytosis, the role of vitamin E deficiency, and common laboratory artifacts that can mimic true disease. With clear explanations and high-quality clinical images, this post offers an easy-to-understand and practical guide to acanthocytosis for doctors, trainees, and medical students.
Questions and Answers:
What is acanthocytosis?
Acanthocytosis is a red blood cell disorder characterized by the presence of acanthocytes—spur-shaped erythrocytes with irregular membrane projections caused by abnormal lipid composition of the red cell membrane.
What are acanthocytes (spur cells)?
Acanthocytes are abnormal red blood cells with unevenly distributed, variably sized spicules caused by increased membrane cholesterol content and reduced membrane fluidity.
What causes acanthocytosis?
Acanthocytosis is caused by inherited disorders such as abetalipoproteinemia and neuroacanthocytosis syndromes, as well as acquired conditions including advanced liver cirrhosis, chronic renal failure, severe malnutrition, and hypothyroidism.
What is the difference between acanthocytes and echinocytes?
Acanthocytes have irregular, uneven membrane spicules and represent a true membrane lipid defect, while echinocytes (burr cells) show uniform, evenly spaced projections and usually represent a reversible environmental or metabolic change.
What is chorea-acanthocytosis?
Chorea-acanthocytosis is a rare inherited neurodegenerative disorder characterized by progressive involuntary movements and the presence of acanthocytes on the peripheral blood smear.
How is acanthocytosis related to liver disease?
In advanced liver cirrhosis, altered lipid metabolism increases red cell membrane cholesterol, producing spur cells and leading to hemolytic anemia known as spur cell anemia.
What is the role of vitamin E in acanthocytosis?
In abetalipoproteinemia, vitamin E deficiency leads to progressive spinocerebellar degeneration, peripheral neuropathy, and retinitis pigmentosa in association with acanthocytosis.
Can acanthocytosis cause anemia?
Yes, acanthocytosis commonly leads to hemolytic anemia due to reduced red cell deformability and increased splenic destruction.
What conditions are associated with echinocytes (burr cells)?
Echinocytes are associated with uremia, electrolyte disturbances such as hypomagnesemia and hypophosphatemia, long-distance running, pyruvate kinase deficiency, and blood storage artifacts.
Is acanthocytosis reversible?
Acanthocytosis is usually irreversible because it reflects a fixed structural abnormality in red cell membrane lipids, unlike echinocytosis which is typically reversible.
How is acanthocytosis diagnosed?
Acanthocytosis is diagnosed by peripheral blood smear examination demonstrating spur cells with irregular membrane projections, supported by clinical and biochemical evaluation.
What is neuroacanthocytosis?
Neuroacanthocytosis refers to a group of rare disorders characterized by progressive neurological disease and acanthocytosis on blood smear.
References:
de Alarcon PA, Coppes MJ.
Acanthocytosis: Clinical presentation, history, physical examination, and causes. Medscape Reference. Available at: http://emedicine.medscape.com/article/954356-clinical
Bohlega S, Al-Jishi A, Dobson-Stone C, Rampoldi L, Saha P, Murad H, Kareem A, Roberts G, Monaco AP.
Chorea-acanthocytosis: Clinical and genetic findings in three families from the Arabian Peninsula. Movement Disorders. 2003;18(4):403–407.
Siegl C, Hamminger P, Jank H, Ahting U, Bader B, Danek A, et al.
Alterations of red cell membrane properties in neuroacanthocytosis. PLoS ONE. 2013;8(10):e76715. doi:10.1371/journal.pone.0076715
Lux SE, Palmer KJ.
Disorders of the red blood cell membrane. In: Greer JP, Arber DA, Glader B, et al., editors. Wintrobe’s Clinical Hematology. 14th ed. Wolters Kluwer; 2018.
Weatherall DJ, Clegg JB.
Inherited red cell membrane disorders and hemolytic anemia. British Journal of Haematology. 2001;113(1):3–17.
Danek A, Walker RH.
Neuroacanthocytosis syndromes. Journal of Neurology. 2009;256(2):254–260.
Bux J, Behrens G, Jaeger G.
Red cell membrane abnormalities in systemic disease. Blood Reviews. 2000;14(4):157–169.
Keywords:
acanthocytosis, acanthocytes, spur cells, acanthocytosis peripheral blood smear, acanthocytes liver cirrhosis, spur cell anemia, echinocytes vs acanthocytes, burr cells blood smear, neuroacanthocytosis, chorea-acanthocytosis, abetalipoproteinemia, vitamin E deficiency neuropathy, retinitis pigmentosa acanthocytosis, red cell membrane lipid disorder, hemolytic anemia spur cells, alcoholic liver cirrhosis blood film, chronic kidney disease echinocytosis, pyruvate kinase deficiency echinocytes, EDTA artifact echinocytes, peripheral smear red cell morphology, inherited acanthocytosis, acquired acanthocytosis, neurological complications of acanthocytosis


Request Online Consultation With Dr M Abdou
Fee: US$100
Secure payment via PayPal (credit and debit cards accepted)
Pay Now