Systemic Mastocytosis

Characteristic urticarial and erythematous lesions on the hands of a patient with systemic mastocytosis.
Systemic Mastocytosis (SM): Symptoms, Diagnosis, and Management:
Systemic Mastocytosis (SM) is a rare, complex hematologic neoplasm characterized by the uncontrolled accumulation of atypical mast cells in various internal tissues and organs, most commonly the bone marrow, spleen, liver, and GI tract. This chronic condition primarily affects adults. Because signs and symptoms, such as urticaria pigmentosa and anaphylaxis, vary widely based on organ involvement, understanding the full clinical picture is critical for accurate systemic mastocytosis diagnosis and treatment. The ICD-10 code for systemic mastocytosis is “D47.02“.
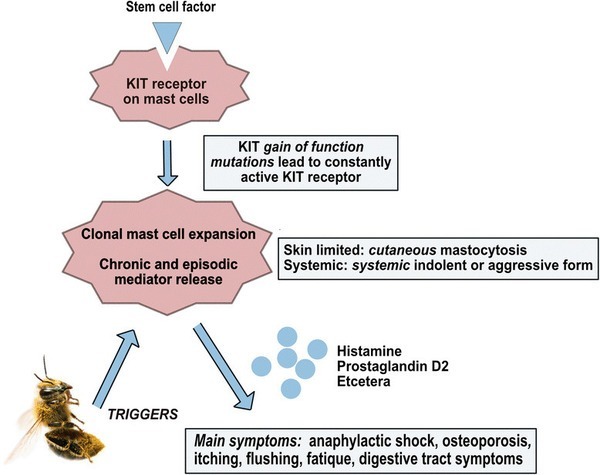
To keep us healthy, mast cells protect our body from foreign threats, such as infections, and help repair its tissues once the threat is gone. As part of their role in the immune system, they create histamine — neurotransmitters that react to those threats and allergens, such as bee stings. Histamine is also released in response to allergens, causing reaction symptoms such as inflammation and even anaphylaxis, a severe, potentially life-threatening kind of reaction.
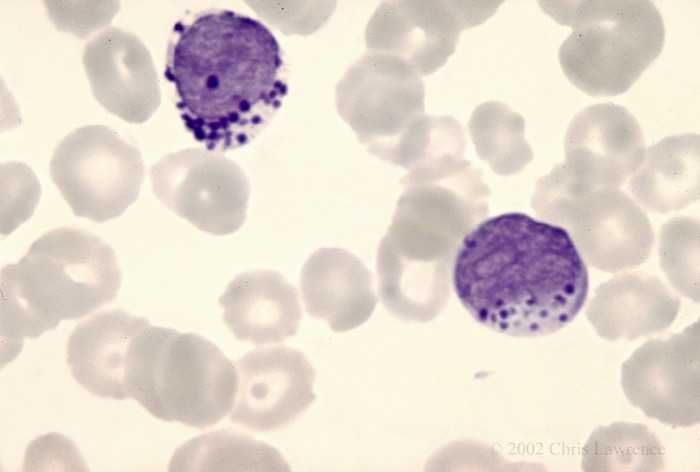
Peripheral blood smear showing circulating atypical mast cells with dense cytoplasmic granules in mast cell leukemia
Mastocytosis is caused by a genetic mutation in which the body accumulates too many mast cells — white blood cells that are part of the immune system and help fight infections.
The World Health Organization (WHO) classification of mastocytosis includes the following:
- Cutaneous mastocytosis – Urticaria pigmentosa, maculopapular cutaneous mastocytosis, diffuse cutaneous mastocytosis, mastocytoma of skin. Cutaneous mastocytosis mainly affects children – where mast cells gather in the skin but are not found in large numbers elsewhere in the body
- Indolent systemic mastocytosis.
- Systemic mastocytosis with an associated (clonal) hematologic non–mast cell lineage disease.
- Aggressive systemic mastocytosis.
- Mast cell leukemia.
- Mast cell sarcoma.
- Extracutaneous mastocytoma.
Mast cells:
Mast cells are produced in the bone marrow, the spongy tissue found in the hollow centers of some bones, and live longer than normal cells. They’re an important part of the immune system and help fight infection.
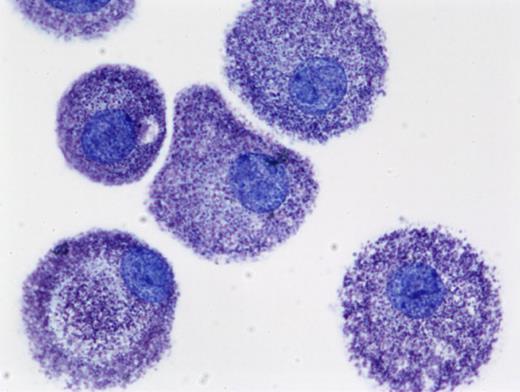
Human mast cells cultured from peripheral blood in the presence of stem cell factor (SCF) and stained with toluidine blue (cytoprep; ×400). Image courtesy of Madeleine K. Radinger
When mast cells detect a substance that triggers an allergic reaction (an allergen), they release histamine and other chemicals into the bloodstream.

Cutaneous mastocytosis in a child presenting with diffuse erythematous maculopapular skin lesions, consistent with mast cell infiltration of the skin
Histamine makes the blood vessels expand and the surrounding skin itchy and swollen. It can also create a build-up of mucus in the airways, which become narrower.
Symptoms of mastocytosis:
The symptoms of mastocytosis can vary depending on the type.
Cutaneous mastocytosis
The most common symptom of cutaneous mastocytosis is abnormal growths (lesions) on the skin, such as bumps and spots, which can form on the body and sometimes blister. The spots are thick and itch when they are hot or if rubbed over it. These spots are known as urticaria pigmentosa.

Pruritus in mastocytosis caused by mast cell mediator release, commonly histamine, leading to itching and skin irritation
Systemic mastocytosis
Some people with systemic mastocytosis may experience episodes of severe symptoms that last 15-30 minutes, often with specific triggers such as physical exertion or stress. Many people do not have any problems.
During an episode you may have:
- skin reactions – such as itching and flushing
- gut symptoms – such as being sick and diarrhea
- muscle and joint pain
- mood changes, headaches, and episodes of tiredness (fatigue)
People with mastocytosis have an increased risk of developing a severe and life-threatening allergic reaction. This is known as anaphylaxis.
The increased risk of anaphylaxis is caused by the abnormally high number of mast cells and their potential to release large amounts of histamine into the blood.
People with mastocytosis may need to carry an adrenaline auto-injector, which can be used to treat the symptoms of anaphylaxis.
There are 3 subtypes of systemic mastocytosis:
- indolent mastocytosis – symptoms are usually mild to moderate and vary from person to person; indolent mastocytosis accounts for around 90% of adult systemic mastocytosis cases.
- aggressive mastocytosis – where mast cells multiply in organs, such as the spleen, liver and digestive system; the symptoms are more wide-ranging and severe, although skin lesions are less common.
- systemic mastocytosis with associated hematological disease – where a condition that affects the blood cells, such as chronic leukemia, also develops.
Causes of mastocytosis:
The cause or causes of mastocytosis are not fully known, but there’s thought to be an association with a change in genes known as the KIT mutation.
The KIT mutation makes the mast cells more sensitive to the effects of a signaling protein called stem cell factor (SCF).
SCF plays an important role in stimulating the production and survival of certain cells, such as blood cells and mast cells, inside the bone marrow.
In very few cases of mastocytosis, it appears the KIT mutation is passed down through families. However, in most cases, the mutation happens for no apparent reason.
Diagnosing mastocytosis:
A physical examination of the skin is the first stage in diagnosing cutaneous mastocytosis.
Your child’s GP or a skin specialist (dermatologist) may rub the affected areas of skin to see if they become red, inflamed and itchy. This is known as Darier’s sign.

Darier’s sign is a hallmark dermatological feature of cutaneous mastocytosis. It is elicited by gently stroking a mastocytosis skin lesion with moderate pressure using a tongue spatula, leading to a localized wheal-and-flare reaction within minutes (arrow). This response reflects mast cell degranulation and is characteristic of urticaria pigmentosa and may also be seen in other forms of cutaneous or systemic mastocytosis.
It’s usually possible to confirm a diagnosis by carrying out a biopsy, where a small skin sample is taken and checked for mast cells.
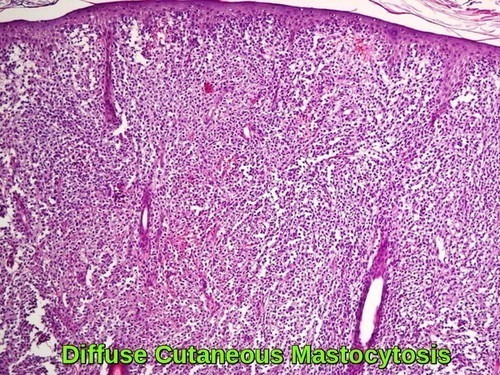
Histopathology of diffuse cutaneous mastocytosis showing dense dermal infiltration by mast cells beneath the epidermis
The following tests are commonly used to look for systemic mastocytosis:
- blood tests – including a full blood count and measuring blood tryptase levels
- an ultrasound scan to look for enlargement of the liver and spleen
- a DEXA scan to measure bone density
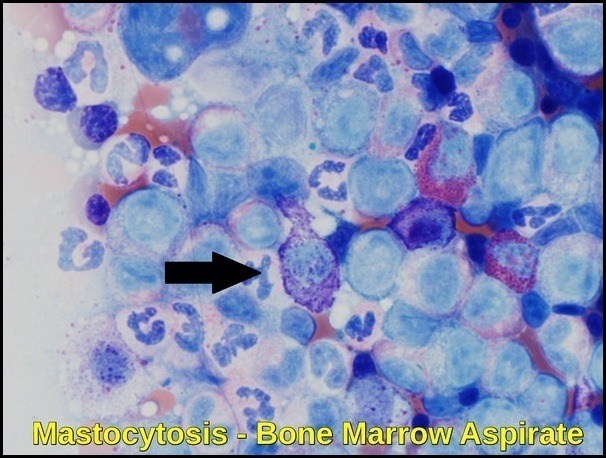
- a bone marrow biopsy test – where a local anesthetic is used and a long needle is inserted through the skin into the bone underneath, usually in the pelvis
A diagnosis of systemic mastocytosis is usually made by finding typical changes on a bone marrow biopsy.
Neoplastic spindle-shaped mast cell with elongated cytoplasmic projections on Wright–Giemsa stain (×100 magnification). The enlarged cell shows hypogranular cytoplasm, a characteristic microscopic feature of systemic mastocytosis and related mast cell neoplasms.
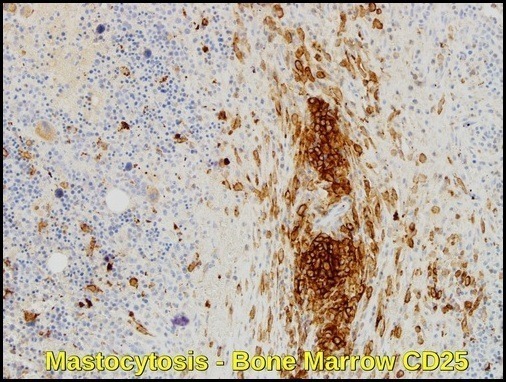
Bone marrow biopsy from a 61-year-old man with indolent systemic mastocytosis showing a dense perivascular mast cell aggregate. CD25 immunohistochemistry (×20) highlights neoplastic mast cells with brown cytoplasmic staining, distinguishing them from normal mast cells. The central aggregate contains predominantly round mast cells, with spindle-shaped forms at the periphery, a characteristic pattern of systemic mastocytosis bone marrow involvement.
Diagnostic Criteria:
The single World Health Organization (WHO) major criterion is multifocal dense infiltrates of mast cells in the bone marrow and/or other extracutaneous organs. One major and 1 minor criterion or 3 minor diagnostic criteria are needed to establish a diagnosis of systemic mastocytosis.
Minor criteria include baseline total tryptase level of greater than 20 ng/mL; greater than 25% of the mast cells in bone marrow aspirate smears or tissue biopsy sections having spindle atypical morphology; mast cells in bone marrow, blood, or other lesional tissue expressing CD25 or CD2; or detection of a codon 816 c-kit point mutation in blood, bone marrow, or lesional tissue.
Treatment:
The treatment of mastocytosis depends on the type, the symptoms of the disease, its extent, and the person’s overall health.
There is no cure for mastocytosis, although several treatments can be used to relieve symptoms and remove a mastocytoma.
Managing symptoms
An important part of treating mastocytosis is controlling a person’s symptoms. One important way to do this is to avoid anything that may cause mast cells to release histamine. This may include extreme temperatures, alcohol, emotional stress, insect bites, and certain medications. For example, nonsteroidal anti-inflammatory drugs (NSAIDs) should be used with caution because these drugs may trigger the release of histamine and can cause severe reactions or an attack.
Doctors may also recommend the following treatments to help relieve mastocytosis symptoms.
Antihistamines. Antihistamines help relieve itching, flushing, and other skin reactions.
Steroids. Steroids may be used to reduce the size of skin lesions.
Epinephrine. People with mastocytosis often carry a syringe of epinephrine, a hormone made by the adrenal glands, in case they need to treat a severe allergic reaction.
Other medications. Other medications can help relieve diarrhea and stomach pain.
Ultraviolet light. Sometimes, exposing the skin rashes to a source of ultraviolet (UV) light can help relieve symptoms of cutaneous mastocytosis.
Surgery. surgery may be performed to remove lesions, such as a mastocytoma.
Targeted therapy. targeted therapy is a treatment that targets the disease’s specific genes, proteins, or the tissue environment unique to mastocytosis that contribute to its growth and survival. This type of treatment blocks the growth of mast cells while limiting damage to healthy cells. Tyrosine kinase inhibitors are a type of targeted therapy. For mastocytosis, the target is the unique protein called the c-kit tyrosine kinase receptor. Treatment with tyrosine kinase inhibitors, including dasatinib (Sprycel), midostaurin (PKC412, recently approved by the FDA for the treatment of systemic mastocytosis), and less commonly imatinib (Gleevec) and nilotinib (Tasigna), may be considered for patients with mast cells that have a mutation in the c-kit tyrosine kinase receptor.
Avapritinib (Ayvakit), a highly selective inhibitor of KIT D816V, was approved by the Food and Drug Administration in 2021 for treatment of advanced systemic mastocytosis (AdvSM) and by the European Medicines Agency in 2022 for AdvSM after prior systemic therapy. The phase 1 EXPLORER and phase 2 PATHFINDER trials demonstrated that avapritinib can elicit complete and durable clinical responses and molecular remission of KIT D816V.

AYVAKIT™ (avapritinib) is a targeted precision therapy approved for adults with advanced systemic mastocytosis (ASM) and unresectable or metastatic gastrointestinal stromal tumors (GIST). This selective tyrosine kinase inhibitor targets KIT D816V mutations, representing a major advance in personalized treatment for mast cell disorders and GIST.
Stem cell transplantation/bone marrow transplantation
A stem cell transplant is a medical procedure in which unhealthy bone marrow is replaced by highly specialized cells, called hematopoietic stem cells, that develop into healthy bone marrow. Hematopoietic stem cells are blood-forming cells found both in the bloodstream and in the bone marrow. Today, this procedure is more commonly called a stem cell transplant, rather than bone marrow transplant, because it is the stem cells in the blood that are typically being transplanted, not the actual bone marrow tissue.
Before recommending transplantation, doctors will talk with the patient about the risks of this treatment and consider several other factors, such as the results of any previous treatment and the patient’s age and general health.
There are 2 types of stem cell transplantation depending on the source of the replacement blood stem cells: allogeneic (ALLO) and autologous (AUTO). ALLO uses donated stem cells, while AUTO uses the patient’s own stem cells. In both types, the goal is to destroy all unhealthy cells in the marrow, blood, and other parts of the body using high doses of chemotherapy and/or radiation therapy and then allow replacement blood stem cells to create healthy bone marrow.
Stem cell transplantation is not used frequently as a treatment for mastocytosis because treatment results are inconsistent and there are significant risks associated with this treatment approach.
Chemotherapy for mastocytosis-related cancer
Chemotherapy is sometimes recommended if mastocytosis becomes cancerous. Chemotherapy is the use of drugs to destroy cancer cells, usually by ending the cancer cells’ ability to grow and divide.
Systemic chemotherapy gets into the bloodstream to reach cancer cells throughout the body. Common ways to give chemotherapy include an intravenous (IV) tube placed into a vein using a needle or in a pill or capsule that is swallowed (orally).
A chemotherapy regimen, or schedule, usually consists of a specific number of cycles given over a set period of time. A patient may receive 1 drug at a time or combinations of different drugs given at the same time.
The side effects of chemotherapy depend on the individual and the dose used, but they can include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhea. These side effects usually go away after treatment is finished.
Getting care for side effects
Mastocytosis treatment often causes side effects. In addition to treatment to manage the condition, an important part of treatment is relieving these side effects. This approach is called palliative or supportive care, and it includes supporting the patient with his or her physical, emotional, and social needs.
Palliative care is any treatment that focuses on reducing symptoms and treatment side effects, improving quality of life and supporting patients and their families. Any person, regardless of age or type of disease, may receive palliative care. It works best when palliative care is started as early as needed in the treatment process.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional support, and other therapies.
Complications of Mastocytosis:
In children, the symptoms of cutaneous mastocytosis usually improve over time but remain stable in adults. In many cases, the condition gets better on its own by the time a child has reached puberty.
The outlook for systemic mastocytosis can vary, depending on the type.
Indolent systemic mastocytosis should not affect life expectancy, but other types can.
A few people develop a serious blood condition, such as chronic leukemia, over their lifetime.
Summary:
Systemic mastocytosis is a rare clonal mast cell disorder characterized by abnormal proliferation and accumulation of mast cells in one or more organs, most commonly the skin, bone marrow, liver, spleen, and gastrointestinal tract. Clinical manifestations are highly heterogeneous, ranging from incidental asymptomatic disease to severe mediator-related symptoms, organ dysfunction, and life-threatening anaphylaxis.
The diagnosis of systemic mastocytosis relies on an integrated assessment of clinical features, bone marrow histopathology, immunophenotyping, and molecular testing, with particular emphasis on KIT mutations, especially KIT D816V. Current World Health Organization (WHO) and International Consensus Classification (ICC) systems categorize systemic mastocytosis into distinct subtypes, including indolent, smoldering, aggressive disease, systemic mastocytosis with an associated hematologic neoplasm, and mast cell leukemia, reflecting prognosis and therapeutic implications.
Management of systemic mastocytosis is individualized according to disease subtype and symptom burden. Treatment ranges from supportive and mediator-targeted therapy, including antihistamines and corticosteroids, to disease-modifying approaches for advanced systemic mastocytosis. Targeted therapies such as tyrosine kinase inhibitors and selective KIT D816V inhibitors, including avapritinib, represent major advances in the personalized treatment of advanced mast cell disorders.
Questions and Answers:
What is systemic mastocytosis?
Systemic mastocytosis is a rare clonal hematologic disorder characterized by abnormal proliferation and accumulation of mast cells in extracutaneous organs, most commonly the bone marrow, liver, spleen, gastrointestinal tract, and skin, leading to mediator-related symptoms and organ dysfunction.
What causes systemic mastocytosis?
Systemic mastocytosis is caused by activating mutations in the KIT gene, most frequently the KIT D816V mutation, which leads to uncontrolled mast cell survival, proliferation, and mediator release.
What are the common symptoms of systemic mastocytosis?
Symptoms vary widely and include flushing, pruritus, urticaria, abdominal pain, diarrhea, anaphylaxis, fatigue, bone pain, cytopenias, hepatosplenomegaly, and osteoporosis, depending on mast cell burden and organ involvement.
How is systemic mastocytosis diagnosed?
Diagnosis is based on World Health Organization criteria incorporating bone marrow histology, immunophenotyping showing aberrant CD25 or CD2 expression on mast cells, molecular detection of KIT mutations, and supportive clinical findings such as elevated serum tryptase.
What are the WHO subtypes of systemic mastocytosis?
WHO classification recognizes indolent systemic mastocytosis, smoldering systemic mastocytosis, aggressive systemic mastocytosis, systemic mastocytosis with an associated hematologic neoplasm, and mast cell leukemia, reflecting disease severity and prognosis.
What is mast cell leukemia?
Mast cell leukemia is the most aggressive form of systemic mastocytosis, defined by a high burden of circulating or bone marrow mast cells, severe organ dysfunction, and poor prognosis, often associated with atypical spindle-shaped mast cells and KIT mutations.
What is Darier’s sign in mastocytosis?
Darier’s sign is a characteristic dermatologic finding in cutaneous mastocytosis, where stroking a skin lesion induces a localized wheal-and-flare reaction due to mast cell degranulation and histamine release.
How is systemic mastocytosis treated?
Treatment is individualized and depends on disease subtype and symptom severity, ranging from antihistamines and mast cell stabilizers for indolent disease to cytoreductive therapy and targeted KIT D816V inhibitors, such as avapritinib, for advanced systemic mastocytosis.
Is systemic mastocytosis curable?
Systemic mastocytosis is generally a chronic condition rather than a curable disease, but modern targeted therapies have significantly improved symptom control, organ function, and survival in patients with advanced disease.
References:
Habashy J, Elston DM. Mastocytosis: Background, pathophysiology, and etiology. Medscape. Available at: https://emedicine.medscape.com/article/1057932-overview
National Health Service (NHS). Mastocytosis: overview, symptoms, and treatment. Available at: https://www.nhs.uk/conditions/mastocytosis/
Patnaik MM, Rindos M, Kouides PA, Tefferi A, Pardanani A. Systemic mastocytosis: a concise clinical and laboratory review. Archives of Pathology & Laboratory Medicine. 2007;131(5):784–791
Valent P. Diagnostic evaluation and classification of mastocytosis. Immunology and Allergy Clinics of North America. 2006;26(3):515–534
Horny HP, Sotlar K, Valent P. Mastocytosis: state of the art. Pathobiology. 2007;74(2):121–132
Metcalfe DD. Mast cells and mastocytosis. Blood. 2008;112(4):946–956. doi:10.1182/blood-2007-11-078097
Broesby-Olsen S, et al. Multidisciplinary management of mastocytosis: Nordic expert group consensus. Acta Dermato-Venereologica. 2016;96. doi:10.2340/00015555-2325
Dana-Farber Cancer Institute. Mastocytosis: what is it and how is it treated? Available at: https://blog.dana-farber.org/insight/2017/12/mastocytosis-treatment/
Bustamante D, George TI. Bone marrow biopsy evaluation for mast cell disorders. The Mastocytosis Society (TMS). Available at: https://tmsforacure.org/expert-information/bone-marrow-biopsy-evaluation-mast-cell-disorders/
Cancer.Net (ASCO). Mastocytosis: treatment options. Available at: https://www.cancer.net/cancer-types/mastocytosis/treatment-options
Gotlib J, Reiter A, DeAngelo DJ. Avapritinib for advanced systemic mastocytosis. Blood. 2022;140(15):1667–1673. doi:10.1182/blood.2021014612
Clinical Trials Arena. AYVAKIT (avapritinib) for the treatment of gastrointestinal stromal tumours (GISTs). Available at: https://www.clinicaltrialsarena.com/projects/ayvakit-avapritinib/
Wikipedia. Mast cell leukemia: peripheral blood smear image. Available at: https://en.wikipedia.org/wiki/Mast_cell_leukemia (accessed December 2, 2015)
Keywords:
systemic mastocytosis, systemic mastocytosis symptoms, systemic mastocytosis diagnosis, systemic mastocytosis treatment, systemic mastocytosis prognosis, systemic mastocytosis hematology, systemic mastocytosis bone marrow biopsy, systemic mastocytosis tryptase, systemic mastocytosis KIT D816V, KIT D816V mutation systemic mastocytosis, indolent systemic mastocytosis, smoldering systemic mastocytosis, aggressive systemic mastocytosis, systemic mastocytosis with associated hematologic neoplasm, mast cell leukemia, mast cell leukemia blood smear, mast cell leukemia diagnosis, mast cell neoplasms, mast cell disorder, mast cell disease symptoms, mastocytosis, mastocytosis symptoms, mastocytosis diagnosis, mastocytosis treatment, mastocytosis rash, mastocytosis skin lesions, cutaneous mastocytosis, diffuse cutaneous mastocytosis, urticaria pigmentosa, Darier’s sign, mastocytosis itching, mastocytosis pruritus, mastocytosis in adults, mastocytosis in children, mastocytosis anaphylaxis, mastocytosis histology, mastocytosis immunohistochemistry CD25, mastocytosis CD117 tryptase, avapritinib systemic mastocytosis, AYVAKIT avapritinib, targeted therapy mastocytosis, tyrosine kinase inhibitor mastocytosis, personalized treatment mastocytosis, what is systemic mastocytosis, how is systemic mastocytosis diagnosed, systemic mastocytosis treatment options






Very nice informative and impressive post you have written, this is quite interesting and i have went through it completely, an upgraded information is shared, keep sharing such valuable information.
I am battling this right now. I have been sick for a very long time. But progressively worse in the past 6 months. Which is when my skin started displaying the symptoms and a dermatologist was finally able to identify it. Unfortunately, I am just now starting the systemic dx process and it could take awhile. With an upped dosage of my h1 and h2, adding singular, my rash is still uncontrollable and the brown spots are also starting to take over my body. I cannot find a lot of information about treating the skin and mixed information about if the spots and rash stay forever. Is there a more effective treatment to target these symptoms specifically? Will the spots stay forever? Should the itchyness and rash fade once I get stabalized with right medications? Unfortunately, I have not been able to come across many doctors who are well versed in mast cell disorders. So I am desperately researching and trying to reach out to anyone who can help.
Hi Kristin,
Thanks for your comment.
I totally understand your frustration caused by the itchiness and the disfiguring skin rash.
However, there is some piece of information missing in your comment regarding the diagnosis of systemic mastocytosis made by your dermatologist:
1- How high is your blood tryptase level?
2- Have you had an abdominal ultrasound scan?
3- Have you had a bone marrow biopsy?
4- Have you had a trial of systemic steroids?
Looking forward to having your answers to better understand and advise regarding your disease.
BW,
My wife, 66, was recently diagnosed with systemic mastocytosis. This article has been extremely helpful in preparing us for our first consult with a hemotologist. Many thanks Dr. Abdou.
Hi Jason,
Thank you for taking the time to reach out to me.
I really appreciate your kind words.
I also want to extend my best wishes to your wife for a speedy recovery.
Take care and all the best.
M Abdou