Langerhan’s Cell Histiocytosis
Langerhans Cell Histiocytosis (LCH), historically referred to as Histiocytosis X, represents a spectrum of clonal dendritic cell disorders ranging from the typically localized and indolent unifocal eosinophilic granuloma to the more aggressive multifocal form and the fulminant disseminated variant previously known as Letterer–Siwe disease, which carries a high risk of morbidity and mortality. This heterogeneous group of conditions is characterized by pathological proliferation of Langerhans cells that can affect bone, skin, lymph nodes, lungs, and other organs, leading to variable clinical presentations and outcomes.
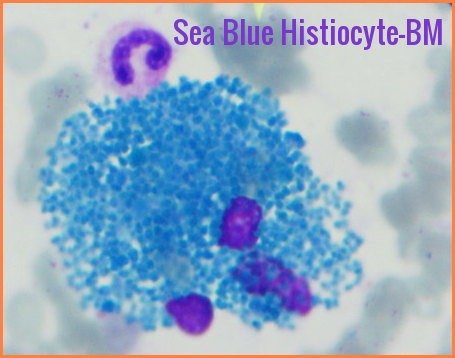
This disorder is characterized by an abnormal increase in certain immune cells called histiocyte cells. Histiocyte cells are a form of white blood cells that help the immune system destroy foreign materials and fight infection. The extra immune cells produced by this condition may form tumors with infiltration into organs locally or diffusely.
Langerhans cell histiocytosis historically was thought of as a cancer-like condition, but more recently researchers have begun to consider it an autoimmune phenomenon in which immune cells begin to overproduce and attack the body instead of fighting infection.
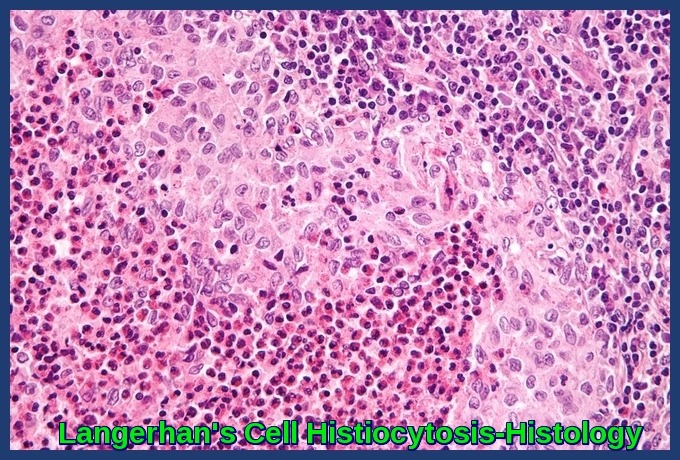
Langerhans Cell Histiocytosis histology demonstrating clusters of atypical Langerhans cells with eosinophils.
Most cases affect children between 1 and 15 years old, with the majority of new cases in children between 5 and 10.

High-risk multisystem Langerhans Cell Histiocytosis in a 22-month-old boy presenting with extensive cutaneous involvement.
Langerhan’s Cell Histiocytosis provokes a non-specific inflammatory response, which includes fever, lethargy, and weight loss. Organ involvement can also cause more specific symptoms.
Manifestations may include lung infiltrates; bone lesions; skin rashes; and hepatic, hematopoietic, and endocrine dysfunction.
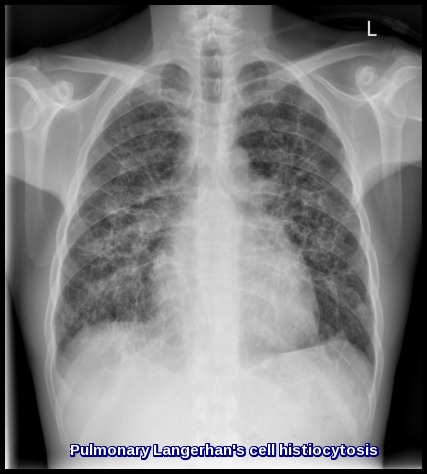
Pulmonary Langerhans Cell Histiocytosis presenting with bilateral reticulonodular infiltrates on chest X-ray.
Diagnosis is based on biopsy.
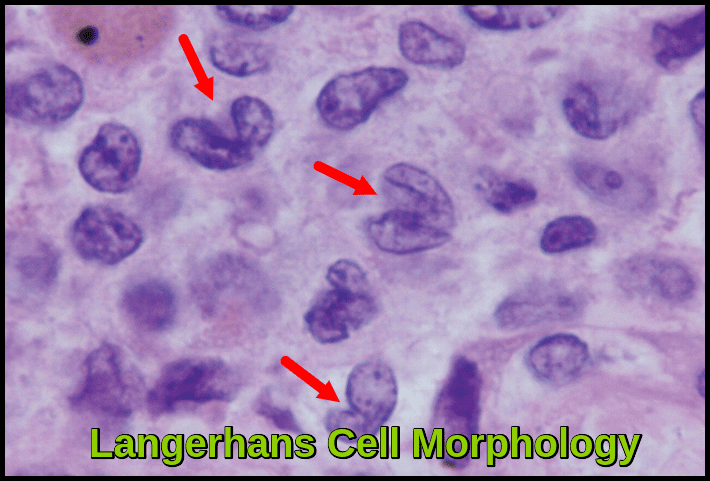
Oil immersion photomicrograph (×1200, H&E stain) showing Langerhans cells with irregular deeply grooved “coffee-bean” nuclei and indistinct cell borders, characteristic of Langerhans Cell Histiocytosis.
Factors predicting a poor prognosis include age < 2 yr and dissemination, particularly involving the hematopoietic system, liver, lungs, or a combination.
Treatment includes supportive measures, chemotherapy, local treatment with surgery or radiation therapy as indicated by the extent of disease.
Systemic chemotherapy is indicated for multisystem disease and cases of single-system disease not responsive to other treatment. The combination of cytotoxic drugs and systemic steroids is generally effective. Low-to-moderate doses of methotrexate, prednisone, and vinblastine are used.
Some patients require hormone replacement for diabetes insipidus (DDAVP) or other manifestations of hypopituitarism.
Summary:
Langerhans Cell Histiocytosis (LCH) is a rare clonal dendritic cell disorder characterized by pathological proliferation of CD1a+/CD207+ Langerhans cells driven in many cases by MAPK pathway mutations such as BRAF-V600E. The disease presents with a wide spectrum of clinical manifestations, ranging from isolated bone or skin lesions to high-risk multisystem involvement affecting the liver, spleen, hematopoietic system, and lungs. Diagnosis relies on histopathology, immunophenotyping, and radiologic evaluation, while treatment strategies include corticosteroids, vinblastine-based regimens, targeted therapies such as BRAF and MEK inhibitors, and supportive organ-specific care. Early recognition and accurate risk stratification are essential, as prognosis varies significantly between single-system and high-risk multisystem disease. This comprehensive review summarizes pathogenesis, clinical features, diagnostic criteria, and evidence-based management of Langerhans Cell Histiocytosis to support improved clinical practice.
Questions and Answers:
What is Langerhans Cell Histiocytosis (LCH)?
Langerhans Cell Histiocytosis is a rare clonal dendritic cell disorder characterized by the proliferation of CD1a+/Langerin+ Langerhans cells, often driven by MAPK pathway mutations such as BRAF-V600E. It may present as single-system or multisystem disease with variable severity.
What causes Langerhans Cell Histiocytosis?
LCH is caused by somatic mutations—most commonly BRAF-V600E or MAP2K1—that activate the MAPK–ERK pathway, leading to uncontrolled proliferation of Langerhans cells. These mutations support the concept of LCH as an inflammatory myeloid neoplasm.
What are the typical skin manifestations of Langerhans Cell Histiocytosis?
Skin involvement often appears as erythematous papules, crusted lesions, seborrheic dermatitis-like eruptions on the scalp, or widespread rash on the trunk. Infants frequently present with diffuse papulonodular lesions or ulcerative plaques as shown in the clinical images.
How does multisystem Langerhans Cell Histiocytosis present in children?
High-risk multisystem LCH in infants and young children may involve skin, liver, spleen, bone marrow, and lymph nodes, with symptoms including rash, hepatosplenomegaly, cytopenias, fever, bone pain, and failure to thrive. Early recognition is critical for prognosis.
What are the characteristic radiological findings in pulmonary Langerhans Cell Histiocytosis?
Pulmonary LCH typically shows upper- and mid-zone predominant reticulonodular opacities, cysts, and nodules on imaging. Chest X-ray may reveal diffuse infiltrates, while HRCT is more sensitive for identifying cystic changes.
How is Langerhans Cell Histiocytosis diagnosed?
Diagnosis is based on histology demonstrating Langerhans cells with grooved nuclei, accompanied by eosinophils. Immunohistochemistry confirms CD1a and Langerin (CD207) positivity. Molecular testing for BRAF and MAP2K1 mutations supports classification and treatment planning.
What does Langerhans Cell Histiocytosis look like on histology?
Histology typically shows sheets of Langerhans cells with coffee-bean-shaped nuclei, mixed inflammatory infiltrate rich in eosinophils, and variable fibrosis. These features are well demonstrated in the histology images included in the post.
What are the treatment options for Langerhans Cell Histiocytosis?
Treatment depends on disease extent. Options include corticosteroids, vinblastine-based chemotherapy, cytarabine, cladribine, and targeted therapies such as BRAF or MEK inhibitors for mutation-positive disease. High-risk multisystem cases often require intensive systemic therapy.
What is the prognosis of Langerhans Cell Histiocytosis?
Prognosis varies by risk category: single-system disease generally has excellent outcomes, while high-risk multisystem LCH involving liver, spleen, or bone marrow carries higher morbidity and mortality. Mutation status and response to initial therapy are key prognostic indicators.
Can Langerhans Cell Histiocytosis affect the lungs?
Yes, pulmonary involvement may occur in children with multisystem LCH and is especially common in adult smokers as isolated pulmonary LCH. It presents with cough, dyspnea, and characteristic cystic and nodular lung lesions on imaging.
References:
Komp DM. Historical perspectives of Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1987 Mar;1(1):9–21.
Merad M, Ginhoux F, Collin M. Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nat Rev Immunol. 2008 Dec;8(12):935–947.
Egeler RM, van Halteren AG, Hogendoorn PC, Laman JD, Leenen PJ. Langerhans cell histiocytosis: fascinating dynamics of the dendritic cell–macrophage lineage. Immunol Rev. 2010 Mar;234(1):213–232.
Asri E, Gustia R, Raflis Y, Izzah AZ, Zagoto YES, Sari II. A Case of High-Risk Multisystem Langerhans Cell Histiocytosis in a 22-Month-Old Boy. In: Arcangeli F, Lotti TM, editors. Clinical Cases in Neonatal and Infant Dermatology. Clinical Cases in Dermatology. Springer, Cham; 2022. https://doi.org/10.1007/978-3-030-91523-0_5
Abbott GF, Rosado-de-Christenson ML, Franks TJ, Frazier AA, Galvin JR. From the Archives of the AFIP: Pulmonary Langerhans cell histiocytosis. RadioGraphics. 2004;24(3):821–841. doi:10.1148/rg.243045005.
Keywords:
Langerhans Cell Histiocytosis, LCH, multisystem LCH, single-system LCH, high-risk LCH, pediatric Langerhans Cell Histiocytosis, infant LCH rash, Langerhans cells microscopy, coffee-bean nuclei, LCH histology, LCH skin lesions, LCH scalp lesions, pulmonary Langerhans Cell Histiocytosis, LCH X-ray findings, BRAF V600E LCH, MAPK pathway mutations LCH, dendritic cell neoplasm, eosinophilic granuloma, Letterer-Siwe disease, bone lesions LCH, dermatologic LCH, multisystem histiocytosis, LCH diagnosis, CD1a Langerin CD207, LCH treatment, vinblastine prednisone LCH, targeted therapy BRAF inhibitors, MEK inhibitors LCH, LCH prognosis, childhood histiocytosis, neonatal histiocytosis, LCH clinical features, LCH management guidelines.





Hey, It really is an incredibly fantastic and informative website. Good to discover your site Very well article! I’m simply in love with it.