Lymphatic Filariasis
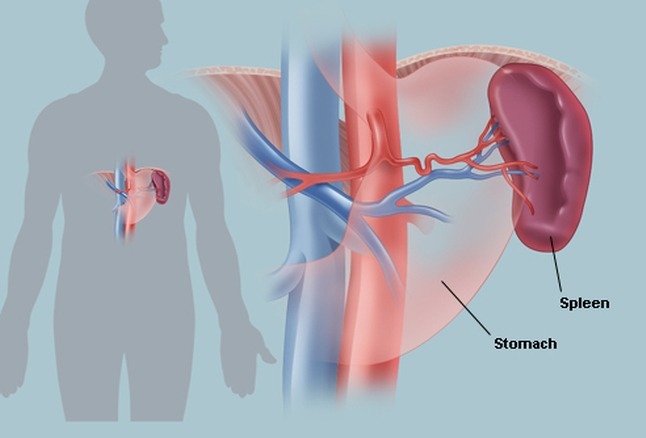
Lymphatic filariasis is a mosquito-borne parasitic infection classified as a neglected tropical disease (NTD) and caused by microscopic thread-like filarial worms that reside in the human lymphatic system. This system is essential for maintaining fluid homeostasis and immune defence, and chronic infection can lead to significant lymphatic dysfunction. Transmission occurs when infected mosquitoes introduce larval parasites (microfilariae) into the bloodstream, allowing the worms to mature within lymphatic vessels and potentially cause long-term complications such as lymphedema and elephantiasis.
Individuals affected by lymphatic filariasis may develop chronic lymphedema, progressive elephantiasis, and in men, scrotal swelling known as hydrocele. The condition is one of the world’s leading causes of long-term disability, with significant physical and psychosocial consequences. Disfigurement often leads to stigma and social exclusion, particularly for women, and the resulting functional impairment can limit a person’s ability to work, creating substantial economic and emotional burdens on families and entire communities.
The World Health Organization (WHO) has identified lymphatic filariasis as the second leading cause of permanent and long-term disability in the world, after leprosy.
The WHO acknowledges the achievement of the Republic of Yemen for eliminating lymphatic filariasis as a public health problem, making it the second country, after Egypt, in WHO’s Eastern Mediterranean Region to achieve the criteria.
Lymphatic Filariasis is caused by Wuchereria bancrofti, Brugia malayi, and Brugia timori.
Transmission is by mosquitoes. Infective larvae from the mosquito migrate to the lymphatics, where they develop into threadlike adult worms within 6 to 12 mo. Females are 80 to 100 mm long; males are about 40 mm long. Gravid adult females produce microfilariae that circulate in the blood.
Current estimates suggest that about 120 million people are infected.
Clinical features:
Infection can result in microfilaremia without overt clinical manifestations. Symptoms and signs are caused primarily by adult worms. Microfilaremia gradually disappears after people leave the endemic area.
Acute inflammatory filariasis
Consists of recurrent episodes of fever and inflammation of lymph nodes with lymphangitis or acute epididymitis and spermatic cord inflammation. Localized involvement of a limb may cause an abscess that drains externally and leaves a scar. ADL is often associated with secondary bacterial infections. ADL episodes usually precede
Localized involvement of a limb may cause an abscess that drains externally and leaves a scar. Acute adenolymphangitis is often associated with secondary bacterial infections.
Acute filariasis is more severe in previously unexposed immigrants to endemic areas than in native residents.
Chronic filarial disease
Develops insidiously after many years. In most patients, asymptomatic lymphatic dilation occurs, but chronic inflammatory responses to adult worms and secondary bacterial infections may result in chronic lymphedema of the affected body area. Increased local susceptibility to bacterial and fungal infections further contributes to its development.
Chronic pitting lymphedema of a lower extremity can progress to elephantiasis (chronic lymphatic obstruction).
W. bancrofti can cause hydrocele and scrotal elephantiasis. Other forms of the chronic filarial disease may lead to chyluria and chyloceles.
Extralymphatic signs
Include chronic microscopic hematuria and proteinuria and mild polyarthritis, all presumed to result from immune complex deposition.
Tropical pulmonary eosinophilia
Uncommon manifestation with recurrent bronchospasm, transitory lung infiltrates, low-grade fever, and marked eosinophilia. It is most likely due to hypersensitivity reactions to microfilariae. It can lead to pulmonary fibrosis.
Diagnosis:
The traditional diagnostic method for filariasis is to demonstrate microfilariae in the peripheral blood or skin.
Blood samples must be obtained when microfilaremia peaks (at night where W. bancrofti is endemic, but during the day where B. malayi and B. timori occur).

Left: Wuchereria bancrofti microfilaria on a Giemsa-stained thick blood smear. Right: Brugia malayi microfilaria on a Giemsa-stained thick smear. Center: Female Aedes aegypti mosquito feeding, illustrating the vector responsible for transmitting filariasis.
Several blood tests are available:
Antigen detection: A rapid-format immunochromatographic test for W. bancrofti antigens
Molecular diagnosis: Polymerase chain reaction assays for W. bancrofti and B. malayi
Antibody detection: Alternatively, enzyme immunoassay tests for antifilarial IgG1 and IgG4
Patients with active filarial infection typically have elevated levels of antifilarial IgG4 in the blood.
Microfilariae may also be observed in chylous urine and hydrocele fluid. If lymphatic filariasis is suspected, urine should be examined macroscopically for chyluria and then concentrated to examine for microfilariae.
Diethylcarbamazine (DEC) kills microfilariae and a variable proportion of adult worms. DEC 2 mg/kg po tid for 12 days is typically given; 6 mg/kg po once is an alternative.
Adverse effects with DEC are usually limited and depend on the number of microfilariae in the blood. The most common are dizziness, nausea, fever, headache, and pain in muscles or joints, which are thought to be related to release of filarial antigens.
Before initiating treatment, patients should be evaluated for possible co-infection with Loa loa or Onchocerca volvulus, as administration of diethylcarbamazine (DEC) in these settings can trigger severe adverse reactions due to rapid parasite killing.
A single dose of albendazole 400 mg po plus either ivermectin (200 mcg/kg po) in areas where onchocerciasis is co-endemic or DEC (6 mg/kg) in areas without onchocerciasis and loiasis rapidly reduces microfilaremia levels, but ivermectin does not kill adult worms. A number of drug combinations and regimens have been used in mass treatment programs.
Also, doxycycline has been given long-term (eg, 100 mg po bid for 4 to 8 wk). Doxycycline kills certain bacteria within filaria, leading to the death of the worms.
Chronic lymphedema requires meticulous skincare, including the use of systemic antibiotics to treat secondary bacterial infections; these antibiotics may slow or prevent progression to elephantiasis. Whether DEC therapy prevents or lessens chronic lymphedema remains controversial. Conservative measures such as elastic bandaging of the affected limb reduce swelling. Surgical decompression using nodal-venous shunts to improve lymphatic drainage offers some long-term benefit in extreme cases of elephantiasis. Massive hydroceles can also be managed surgically.
Prevention:
Fifteen countries are now acknowledged for achieving elimination of lymphatic filariasis as a public health problem.
Avoiding mosquito bites in endemic areas is the best protection.
Chemoprophylaxis with DEC or combinations of antifilarial drugs can suppress microfilaremia and thereby reduce transmission of the parasite by mosquitoes in endemic communities.
DEC has even been used as an additive to table salt in some endemic areas.
Summary:
Filariasis is a mosquito-borne parasitic infection caused primarily by Wuchereria bancrofti and Brugia malayi, leading to chronic lymphatic dysfunction and significant global morbidity. Transmission occurs when infected mosquitoes introduce microfilariae into the human bloodstream, where they migrate to the lymphatic system and mature into adult worms. Long-standing infection can result in lymphedema, elephantiasis, and hydrocele, making lymphatic filariasis one of the leading causes of permanent disability worldwide. Diagnosis relies on clinical features, microfilariae detection on blood smears, antigen testing, and imaging for lymphatic involvement. Effective treatment includes antifilarial therapy such as diethylcarbamazine (DEC), ivermectin, and albendazole, alongside vector-control strategies and morbidity-management programs to prevent long-term complications. Comprehensive control initiatives led by the WHO aim to eliminate filariasis as a public health problem through mass drug administration (MDA) and improved surveillance. This post provides an in-depth overview of the etiology, pathogenesis, clinical manifestations, diagnosis, laboratory findings, and current treatment and prevention strategies for lymphatic filariasis.
Questions and Answers:
What is filariasis and how is it transmitted?
Filariasis is a mosquito-borne parasitic infection caused by thread-like filarial worms such as Wuchereria bancrofti and Brugia malayi. Transmission occurs when infected mosquitoes introduce microfilariae into the bloodstream during a blood meal.
What are the main symptoms of lymphatic filariasis?
Common symptoms include lymphedema, recurrent bacterial infections, progressive elephantiasis, and in men, hydrocele due to chronic lymphatic obstruction.
Which parasites cause lymphatic filariasis?
The primary causative agents are Wuchereria bancrofti, Brugia malayi, and less commonly Brugia timori, all of which infect the lymphatic system and can lead to long-term disability.
How is filariasis diagnosed in clinical practice?
Diagnosis is based on detecting microfilariae in thick or thin blood smears, antigen detection tests, PCR methods, and imaging to assess lymphatic involvement.
What does a microfilaria look like on a blood smear?
A microfilaria appears as a slender, motile, thread-like larval worm on a Giemsa-stained thick blood smear, often surrounded by scattered blood cells.
Which mosquito species transmits filariasis?
Several mosquito genera act as vectors, most notably Aedes, Anopheles, Culex, and Mansonia, with Aedes aegypti commonly implicated in endemic regions.
How does chronic filariasis lead to lymphedema and elephantiasis?
Adult worms residing in lymphatic vessels cause obstruction, inflammation, and fibrosis, resulting in impaired lymphatic drainage and progressive tissue swelling.
What treatments are available for lymphatic filariasis?
Diethylcarbamazine (DEC), ivermectin, and albendazole are standard antifilarial therapies, often used in combination during mass drug administration (MDA) programs.
Why must patients be screened for Loa loa before receiving DEC?
Co-infection with Loa loa can lead to severe inflammatory reactions when DEC is administered, due to the rapid killing of microfilariae, necessitating careful pre-treatment assessment.
Can filariasis cause long-term disability?
Yes. Chronic lymphatic obstruction can result in permanent lymphedema, elephantiasis, and hydrocele, significantly affecting mobility, social functioning, and quality of life.
How can filariasis be prevented in endemic areas?
Prevention strategies include mosquito control, use of insecticide-treated nets, annual mass drug administration, early diagnosis, and morbidity-management programmes to prevent long-term complications.
Is filariasis curable?
Antifilarial therapy can kill microfilariae and reduce transmission, but advanced lymphedema or elephantiasis may be irreversible, requiring lifelong supportive care.
What is the global burden of lymphatic filariasis?
Filariasis remains a major public health challenge in many tropical and subtropical regions and is recognised by WHO as one of the leading causes of permanent disability worldwide.
References:
Centers for Disease Control and Prevention (CDC). Lymphatic Filariasis: Epidemiology, Clinical Features, and Treatment. Available at: https://www.cdc.gov/parasites/lymphaticfilariasis/index.html
World Health Organization (WHO). Yemen Eliminates Lymphatic Filariasis Despite Ongoing Challenges. Available at: https://www.who.int/neglected_diseases/news/yemen-eliminates-lymphatic-filariasis/en/
World Health Organization (WHO). Lymphatic Filariasis: Global Epidemiology, Transmission, and Public Health Impact. Available at: https://www.who.int/health-topics/lymphatic-filariasis
Centers for Disease Control and Prevention (CDC). Parasites – Lymphatic Filariasis: Diagnostic Methods and Management Guidelines. Available at: https://www.cdc.gov/parasites/lymphaticfilariasis/
Ottesen EA. Lymphatic filariasis: treatment, control, and strategies for elimination. Adv Parasitol. 2006;61:395–441.
Bockarie MJ, Deb RM. Elimination of lymphatic filariasis: current status, barriers, and global progress. Curr Opin Infect Dis. 2010;23(6):563–568.
Michael E, Bundy DAP, Grenfell BT. Reassessing the global prevalence and disease burden of lymphatic filariasis. Lancet. 1996;348(9027):103–105.
Keywords:
filariasis, lymphatic filariasis, microfilariae, Wuchereria bancrofti, Brugia malayi, mosquito-borne parasitic infection, elephantiasis, lymphedema, hydrocele, thick blood smear microfilaria, filarial worms, Aedes aegypti mosquito, filariasis diagnosis, filariasis treatment, diethylcarbamazine DEC, ivermectin albendazole therapy, mass drug administration MDA, WHO filariasis elimination, Loa loa screening, Onchocerca volvulus risk, filariasis transmission cycle, global burden of filariasis, parasitic disease lymphatic system, filariasis prevention, endemic filariasis regions, microscopy Giemsa stain filariasis