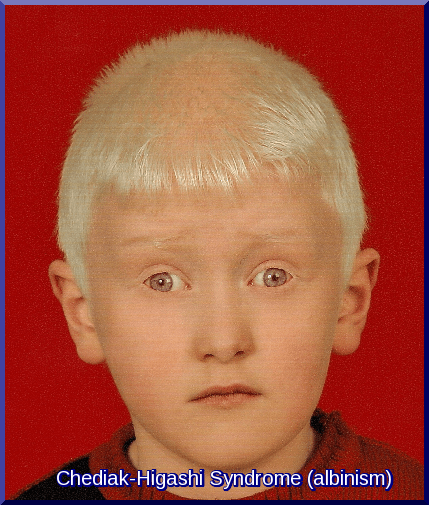
Chediak-Higashi Syndrome
Chediak-Higashi Syndrome (CHS) is a very rare autosomal recessive primary immunodeficiency disorder characterized by a complex mutation in a lysosomal trafficking regulator protein. This mutation severely impairs the immune system’s function (phagocytosis and bacterial lysis), leading to devastating consequences for the patient, including recurrent bacterial infections (especially respiratory), partial albinism, an increased bleeding tendency, and often progressive neurological disease.
While the condition may initially present with features of albinism, the persistent and severe recurrent infections are the key clinical sign that should prompt an investigation for Chediak-Higashi Syndrome. A positive family history is a known risk factor, but it is uncommon. Definitive diagnosis is confirmed through identifying characteristic giant granules in white blood cells and genetic testing for the underlying mutation.
Diagnosis of Chediak-Higashi syndrome (CHS) is made by Genetic testing and recognising the characteristic giant granules in neutrophils, eosinophils, and other cells (e.g. lymphocytes, melanocytes, neural Schwann cells).
Bone marrow smears reveal giant inclusion bodies in leukocyte precursor cells.
Laboratory findings include neutropenia and hypergammaglobulinemia.
Infants born with Chediak-Higashi syndrome (CHS) have nonpigmented skin (similar to albinos but in patchy distribution), blonde hair, and blue eyes.
Signs and symptoms include the following:
- Lymphadenopathy
- Enlarged liver and spleen
- Jaundice
- Albinism, impaired vision, photophobia
- Aphthae (a small, shallow, painful ulceration that usually affects the oral mucosa, but not underlying bone. Aphthae occasionally may affect other body tissues, including those of the GI tract and the external genitals. They do not appear to be infectious, contagious, or sexually transmitted)
- Gingivitis
- Hyperhidrosis (a condition characterized by excessive sweating)
- Miliaria (skin disease marked by small and itchy rashes)
- Severe and extensive pyoderma
- Recurrent sinopulmonary infections
- Fever unrelated to recognizable infection
- Epilepsy
- Mental retardation
- Ataxia causing incoordination and a typical ataxic gait
- Tremor
- Peripheral neuropathy causes motor and sensory changes and weakness (if the patient survives into adulthood)
Case Report:
A 2-year-old girl presented with recurrent infections, hepatosplenomegaly, and photophobia. On examination, she had blond hair with a metallic sheen. The blood smear showed giant lysosomes in the white blood cells and a diagnosis of Chediak-Higashi syndrome was made. CHS is a rare autosomal recessive disease (gene CHS1/LYST at 1q42.1-2). Giant cytoplasmic granules are pathognomonic. Death often occurs before the age of 7 years because of the so-called accelerated phase, with hepatosplenomegaly, lymphadenopathy, and pancytopenia or severe recurrent bacterial infections. The laboratory diagnosis was supported by partial oculocutaneous albinism and typical microscopic granules in hair shafts. A new mutation was identified and the patient was found to be homozygous for a sequence change in the LYST gene.

Blood film showing pathognomonic giant cytoplasmic granules in neutrophils and eosinophils (A), neutrophils (B), and lymphocytes (C, D).
Treatment includes supportive care using antibiotics, interferon-gamma, and sometimes corticosteroids and bone marrow transplantation.
Prophylactic antibiotics can help prevent infections, and interferon-gamma can help restore some immune system function. Pulse doses of corticosteroids and splenectomy sometimes induce transient remission. However, unless bone marrow transplantation is done, most patients die of infections by the age of 7 years.
Hematopoietic Stem Cell Transplantation (HSCT) from an HLA-matched sibling or from an unrelated donor or cord blood transplantation is the treatment of choice to correct the immunologic and hematologic manifestations of early-onset Chédiak-Higashi syndrome (CHS).
Summary:
Chediak–Higashi Syndrome (CHS) is a rare autosomal recessive immunodeficiency caused by pathogenic LYST mutations that disrupt lysosomal trafficking and impair phagolysosome fusion. This defect leads to recurrent bacterial infections, partial oculocutaneous albinism, easy bruising or bleeding, and progressive neurological decline. Blood films show pathognomonic giant cytoplasmic granules in neutrophils, eosinophils, and lymphocytes, a hallmark feature of CHS. Diagnosis relies on characteristic microscopy findings, immunologic evaluation, and genetic testing for LYST mutations. Early hematopoietic stem cell transplantation improves survival, particularly before the accelerated phase develops. Supportive care, infection prophylaxis, and management of neurologic and hematologic complications remain essential.
Questions and Answers:
What causes Chediak–Higashi Syndrome?
CHS is caused by mutations in the LYST gene, which leads to abnormal lysosomal trafficking and defective phagolysosome fusion in immune cells. This results in recurrent infections, albinism, and bleeding problems.
What are the hallmark signs of Chediak–Higashi Syndrome?
The most characteristic signs are partial oculocutaneous albinism, severe recurrent bacterial infections, easy bruising or bleeding, and giant cytoplasmic granules in white blood cells seen on a peripheral blood smear.
How is Chediak–Higashi Syndrome diagnosed?
Diagnosis is based on detecting giant granules in neutrophils, eosinophils, and lymphocytes on blood film, supported by immunologic assessment and molecular testing confirming a LYST mutation.
What do the giant granules in CHS indicate?
These granules reflect defective lysosomal fusion and storage, representing the pathognomonic cellular abnormality of CHS. They impair neutrophil function and contribute to recurrent infections.
Is albinism always present in Chediak–Higashi Syndrome?
Most patients show partial albinism with light hair, pale skin, and light-colored irises, but the degree of pigment dilution can vary.
How is Chediak–Higashi Syndrome treated?
The only curative option is early hematopoietic stem cell transplantation (HSCT), ideally before the accelerated phase. Supportive therapy includes infection prophylaxis, prompt treatment of infections, and management of bleeding tendencies.
What is the accelerated phase of CHS?
The accelerated phase is a life-threatening lymphohistiocytic infiltration resembling HLH (hemophagocytic lymphohistiocytosis), causing fever, hepatosplenomegaly, pancytopenia, and progressive organ failure.
Can Chediak–Higashi Syndrome cause neurological problems?
Yes, progressive neurological decline—such as peripheral neuropathy, ataxia, or cognitive impairment—is common and may continue even after HSCT.
Which microscopic findings help confirm CHS?
Peripheral blood film images show giant cytoplasmic granules within neutrophils, eosinophils, and lymphocytes, which are pathognomonic for the disease.
Is Chediak–Higashi Syndrome related to Griscelli Syndrome?
Both conditions cause pigment dilution and immunodeficiency, but they involve different genes and mechanisms. CHS affects LYST, while Griscelli Syndrome involves RAB27A, MYO5A, or MLPH.
References:
Kaplan J, De Domenico I, Ward D.M. Chediak–Higashi Syndrome. Curr Opin Hematol. 2008; 15(1): 22–29. doi:10.1097/MOH.0b013e3282f2b4c5
Nowicki R.J. Chediak–Higashi Syndrome: Practice Essentials, Background, Pathophysiology. Medscape Reference. Available at: https://emedicine.medscape.com/article/1114607-overview
Delcourt-Debruyne E.M., Boutigny H.R., Hildebrand H.F. Features of Severe Periodontal Disease in a Teenager With Chediak–Higashi Syndrome. J Periodontol. 2000; 71(5): 816–824. doi:10.1902/jop.2000.71.5.816
Liang J.S., Lu M.Y., Tsai M.J., Lin D.T., Lin K.H. Bone Marrow Transplantation From an HLA-Matched Unrelated Donor for Treatment of Chediak–Higashi Syndrome. J Formos Med Assoc. 2000; 99(6): 499–502. PubMed ID 10870324
Nowicki R., Sczarmach S. Chediak–Higashi Syndrome. eMedicine. 2009. https://emedicine.medscape.com/article/1114607-overview
Tanaka T. Chediak–Higashi Syndrome: Abnormal Lysosomal Enzyme Levels in Granulocytes of Patients and Family Members. Pediatr Res. 1980; 14(8): 901–904. doi:10.1203/00006450-198008000-00012
Misra V.P., King R.H., Harding A.E., et al. Peripheral Neuropathy in the Chediak–Higashi Syndrome. Acta Neuropathol (Berl). 1991; 81(3): 354–358. doi:10.1007/BF00293463
Introne W.J., Westbroek W., Golas G.A., et al. Chediak–Higashi Syndrome: Advances in the Understanding of Lysosomal Defects. Expert Rev Clin Immunol. 2015; 11(8): 1097–1111. doi:10.1586/1744666X.2015.1060127
Ménasché G., Feldmann J., Houdusse A., et al. Biochemical and Functional Characterization of Rab27a Mutations Occurring in Griscelli Syndrome Patients. Blood. 2003; 101(7): 2736–2742. doi:10.1182/blood-2002-07-2246
Antunes H., Pereira Â., Cunha I. Chediak–Higashi Syndrome: Pathognomonic Feature. The Lancet. 2013; 381(9873): 1872. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)60020-3/fulltext
Keywords:
Chediak–Higashi syndrome, CHS, LYST gene mutation, lysosomal trafficking regulator, primary immunodeficiency, rare genetic disorder, autosomal recessive disorder, partial oculocutaneous albinism, giant cytoplasmic granules, neutropenia, defective phagocytosis, recurrent bacterial infections, immunodeficiency treatment, bone marrow transplantation, hematopoietic stem cell transplantation HSCT, HSCT for CHS, genetic testing for CHS, CHS diagnosis, CHS symptoms, CHS pathophysiology, CHS management, CHS prognosis, CHS treatment guidelines, lysosomal storage disorder, pediatric immunodeficiency, congenital neutropenia syndrome, lysosomal dysfunction, phagolysosome fusion defect, immunologic disorder, neurological manifestations in CHS, progressive neurodegeneration, albinism with immunodeficiency, hematologic rare diseases, inherited immunodeficiency syndromes, granulocyte function defect, molecular diagnosis of CHS, CHS peripheral neuropathy, CHS periodontal disease, rare hematologic syndromes, immune system genetic disorders, Griscelli Syndrome







Hi
I am writing a text for board review. I find the images used in this resource wonder and I would like to use some of them. I see that it say CC BY-SA 2.0 at the bottom which tells me I could use it even commercially. I write just to confirm.
Hi Talha,
Thank you for your comment.
Please feel free to use the images you need but I would appreciate citing the reference.
Kind regards,
El año pasado un 17 de mayo falleció mi bebe de 6 meses de vida.
Entrando a los 2 meses entro en una fiebre alta que no podíamos controlar y de ahí empezó todo.
Una de las tantas enfermedades tan horribles que se lleva a angelitos.
Padecí de todo estando esos 4 meses internada con ella. La luchamos hasta el final pero quien contra la voluntad de Dios.?
Hello Janet,
I am very sorry to hear about your loss. Losing a child is an unimaginable pain, and my thoughts are with you and your family.
Thank you for sharing your experience, and I hope you continue to find strength and support.
Best regards,
Dr M Abdou